Dr.
Deepak Agrawal
Male
Affiliation
Professor
Department of
Neurosurgery
Contact
Email :
drdeepak@aiims.edu
Phone :
9868398242
Deepak Agrawal
Dr Deepak Agrawal completed his neurosurgical residency training from All India Institute of Medical Sciences, following which he did year long fellowship training in endoscopic and pediatric neurosurgery under Prof Steinbok in Vancouver, Canada. He returned back to India to join AIIMS as faculty.
Dr Agrawal has received training in Gamma-Knife surgery and is a part of the gamma-knife team at AIIMS. He is also trained in stereotactic and image guided neurosurgery and is credited for indigenization of a key component of image-guided neurosurgery which has resulted in more than 99% savings in the cost of disposables used in image-guidance.
Dr Agrawal has a keen interest in research and has been instrumental in securing the ‘DST-FIST’ grant for the department of neurosurgery at AIIMS. He is presently involved in a multinational, muticentric shunt registry and in an autopsy study on diffuse axonal injury which is funded by AIIMS. He has won several national and international awards for his research and has more than 10 chapters in neurosurgical texts and more than 50 publications (including 15 original research articles) which have been published in international publications. His specific research interests are shunt infection and pathogenesis of severe head injury.

Dr.
Manmohan Singh
Male
Affiliation
Professor
Department of
Neurosurgery
Contact
Email :
manmohan1972@gmail.com
mehaknoor@hotmail.com
Phone :
011-26588700
General OPD
Tuesday and Saturday - 9.00 am-1.00pm
Personal Profile:
Born on 9th October 1972. Graduated from Govt. Medical College Amritsar in 1993. Completed internship in 1994 in the same institute. Achieved M.S. (Surgery) degree in 1997 from Post Graduate Institute of Medical Education and Research (PGIMER) Chandigarh and received Silver Medal for topping M.S (Surgery) exam. Thereafter worked as Senior Resident (General Surgery) in PGIMER. Joined AIIMS as MCh Neurosurgery candidate in July 1999 and finished in 2002 May. In June 2003 Joined AIIMS as Assistant Professor Neurosurgery.
Primary area of interest:
Skull base, Vascular and Brachial Plexus surgery apart from Neuro-oncology and spine.
Unit: Neurosurgery unit-II
- Principal investigator in ongoing international multicentric multinational trial: CRASH-2 (A large randomized placebo controlled trail among trauma patients with or at risk of significant haemorrhage, of the effect of antifibrinolytic treatment on death and transfusion requirement) Till now have enrolled 21 patients
- AP12009-G004 in Recurrent Grade III-IV glioma-A multinational and multicentric double blind randomized trial. Sponsored by Antisense Pharma-Germany. Period Dec. 2003 – June 2006 Mahapatra AK, Julka PK, Suri A, Kale SS, Singh Manmohan
- Singh Manmohan, Mahapatra A.K. Pediatric head injury. Asian Archives of Anesthesiology & Resuscitation 2004 (Vol LX 1): March 859-866.
- Singh Manmohan, Mahapatra A.K. Traumatic psudoaneurysm of cavernous internal carotid artery following trans nasal endoscopic decompression of optic nerve. Indian J Neurotrauma. 2004; Vol 1. No.2: 59-61.
- T Rizvi, A Garg, M Singh, M C Sharma. Large intracranial mass with a calcified rim- Is it a brain abscess? Pediatr Neurosurg 2005; 41: 112-114
- Singh M, F U Ahmed, A K Mahapatra. Intraoperative development of contralateral extradural hematoma during evacuation of traumatic acute subdural hematoma_ a rare cause of malignant brain bulge during surgery. Ind J Neurotrauma 2005; vol2(2): 139-140
- Singh Manmohan, F U Ahmed, A K Mahapatra. Traumatic middle meningeal artery pseudoaneurysm causing intracerebral hematoma: a case report and review of literature. Surg Neurol. 2006 Sep; 66(3):321-3; discussion 323.
- Singh Manmohan, Vaishya S, Mehta VS. Economics of head injuries. Neurol India. 2006 Mar; 54(1):78-80
- Manish K Kasliwal, M Singh, A K Mahapatra. Giant cervical pseudomeningocoele following traumatic brachial plexus injury. JOURNAL OF CLINICAL NEUROSCIENCE (A)
- Jain D, Sharma M C, Sarkar C, Gupta D, Singh M, Mahapatra A K. Comparative analysis of diagnostic accuracy of different brain biopsy procedures. Neurol India 2006 Dec; 54(4): 394-398
- D. Jain · M. Sharma · C. Sarkar · V. Suri · A. Garg · M. Singh · B. Sharma · A. Mahapatra. Clear cell Meningioma, an uncommon variant of meningioma: a clinicopathologic study of nine cases. Journal of Neuro-Onology(A)
- A. Mridha · M. Sharma · C. Sarkar · A. Garg · M. Singh · V. Suri Anaplastic ependymoma with cartilaginous and osseous metaplasia: report of a rare case and review of literature Journal of Neuro-Oncology (A)

Dr.
Rajinder Kumar
Male
Affiliation
Professor
Department of
Neurosurgery
Contact
Email :
rklaythalling@rediffmail.com
General OPD
Mondays morning & Thursdays evening
Areas of Interest
- Spine Surgery
- Pediatric
- Endoscopy & Functional neurosurgery
In patient services
daily rounds , operations, consultations
- Role of VIIa in Contusive Brain Injury – A Phase II Trial
- CSF Proteomics Study in Health and Disease
- In Vitro Study of MHC and TGF and Role of Interferon Gamma in Culture of GBM Cells
- Long-term Comparative Study of Anterior versus Posterior Approach in Degenerative Cervical Spondylosis
Four publications are there

Dr.
Ashish Suri
Male
M.B.B.S., M.Ch., D.N.B., M.N.A.M.S.
Affiliation
Professor
Department of
Neurosurgery
Contact
Email :
surineuro@gmail.com
Phone :
26593538
Areas of Interest
Neurosurgery
with special reference to:
Skull base surgery and cerebrovascular surgery:
- Aneurysms: complex and giant
- Arteriovenousmalformations – AVMs
- Cavernomas
- Spinal vascular malformations
- Carotid endartrectomy
- ST-MCA / radial artery bypass
- Moyamoya disease
- Pituitary adenomas
- Acoustic neuromas
- Cavernous sinus lesions
- Petrous and petroclival lesions
- Jugular foramen lesions
- Foramen magnum lesions
- Specialized work in collaboration with ENT and Head& Neck surgery
Endoscopic Neurosurgery
- ETV in hydrocephalus
- Colloid cysts
- Arachnoid cysts
- Neurocysticercosis
- Endonasalendoscopic skull base
- Scope-in scope technique: 4th ventricular lesions
Neuro-Oncology
- Targeted therapy for high grade recurrent gliomas
- Brain tumor banking
Epilepsy Surgery:
- Amygdalo-hippocampectomy
- Corpus callosotomy
- ECOG guided lesionectomy
- Functional hemispherotomy
Spine:
- Craniovertebral junction
- Spinal instrumentation
- Image guided surgery
Neurosurgery Skills Training
Neuro-technology: Virtual Reality Simulation and Neurosurgery Instrumentation
Qualifications &Additional Training:
- 10+2 AISSC, CBSE: Delhi Public School, R.K. Puram, New Delhi
- M.B.B.S.: University College of Medical Sciences, New Delhi.
- M.Ch. Neurosurgery: All India Institute of Medical Sciences, New Delhi.
- Diplomate of National Board - D.N.B. Neurosurgery: National Board of Examinations
- Prof. Vinko V. Dolenc, Ljubljana, Slovenia – Cavernous Sinus & Skull Base Surgery
- Prof. Michael R. Gaab, Greifswald, Germany –Endoscopic Neurosurgery
- Prof. Christopher Wallace, Toronto, Canada - Vascular Neurosurgery
- Prof. Paul Cooper, NYUMC, New York, U.S.A-Image Guided and Endoscopic Spinal Surgery.
- Prof Martin Bettag, Trier, Germany – Endonasal Endoscopic Skull Base Surgery
Clinical and Surgical Experience:
Served for last 20 years at the All India Institute of Medical Sciences, New Delhi.
- Resident – Neurosurgery (Junior, Senior, Chief) – Jan. 1994 to Dec 1999
- Assistant Professor- Neurosurgery: Jan. 2000 to June 2004
- Associate Professor- Neurosurgery: July 2004 to June 2008
- Additional Professor- Neurosurgery: July 2008 to July 2012
- Professor- Neurosurgery: July 2012 till date
Innovations in Clinical Neurosurgery:
Neuro-endoscopy:
- Difficult ETV: new technique
- Colloid cysts: one of the largest series
- Scope-in scope technique: 4th ventricular lesions
- Neuro-endoscopy hands-on skills training: Indo-German collaboration
Skull Base Surgery:
- Dolenc–Kawase rhomboid: modified anterior transpetrosal approach
- Cavernous sinus surgical approaches
- Skills training on skull base approaches: WFNS cadaver workshop
- Skull base endoscopy hands-on workshops: Indo-German collaboration
Cerebrovascular Surgery:
- Complex and giant aneurysms
- Poor grade SAH: NNN therapy
- Skills training on microvascular anastomosis: Carotid Endartrectomy, ST-MCA / Radial artery bypass, Moyamoya disease
- Basic research on vasospasm in SAH
Neuro-oncology:
- Brain tumor banking and molecular definition: collaboration with Neuropathology
- Research on role of AP-12009 (TGF-B2 inhibitor) and Interstitial I 131- ch TNTA/B Mab(COTARA) in recurrent high grade glioma by convection enhanced delivery.
Phrenic nerve stimulation for quadriplegia: first in India
Invited Faculty - International
- The Second International Symposium on the Cavernous Sinus- 20 years later, Ljubljana, Slovenia, September 10-13, 2006.
- 5th International Congress of the World Federation of Skull Base Societies, 19th Annual Meeting of the North American Skull Base Society joint meeting Canada, Vancouver.28 Sept -2 Oct 2008.
- 15th Annual Meeting of the Japanese Society of Neuroendoscopy, 21-22th Nov, 2008 at Tokyo, Japan.
- Conjoint meeting of Congress of Neurological Surgeons (USA) and Neurosurgical Society of India, 24th -29th October 2009, New Orleans, USA.
- 9th Workshop on Transnasal Endoscopic Skull Base Surgery; Trier, Germany from 11th -13thNov. 2009.
- 12th Workshop on Endoscopic Trans-nasal approaches to the Skull Base in the Department of Neurosurgery, Trier, Germany from 4th to 6th May 2011 and Department of Anatomy, University of Mainz, Germany from 2nd to 3rd May 2011.
- 22nd Annual Meeting of North American Skull Base Society, 17th-19th February 2012 at Las Vegas, NV, USA.
- 13th Workshop on Endoscopic Trans-nasal approaches to the Skull Base in the Department of Neurosurgery, Trier, Germany from 9th to 11th May 2012.
- 5th Japan – India Neurosurgery Meeting, Osaka, Japan from 17th to 20th October 2012.
- 15th Hands on Workshop on Endoscopic Trans-nasal approaches to the Skull Base in the Department of Neurosurgery, Trier, Germany from 12th to 14th June 2013.
- XV WFNS World Congress Of Neurosurgery at Seoul South Korea Form 8th to 13th September 2013.
Invited Faculty – National
Various CMEs/ Workshops/ Conferences
Conference organization:
Organizing Secretary of following conferences:
9th Annual Conference of the Skull Base Surgery Society of India and International Skull Base CME and WFNS Microsurgery & Endoscopy Skull Base Cadaver Workshop (Oct. 2007)
Annual Conference of Delhi Neurological Association 2009 – DNACON 2009 (Feb. 2009)
11th Annual Conference of the Indian Society of Cerebrovascular Surgery, International
CME, 8th, 9thOctober, 2011, Pre- Conference Live Neurosurgery and Neuro-intervention
Workshop, 6th, 7thOctober, 2011.
Secretary: DBT Indo-German Neurosurgery Skills Training Workshops.
Secretary : ICMR funded Neurosurgery Skills Training Workshops
Member, Organizing Committee of following conferences
- International Neuroscience Update (1998)
- 1st Mid- annual Conference of Neurosurgical Society of India - Mid-Neurocon (2002)
- Annual Indo-Japanese Neurosurgery Conference (2003)
- 3rd Annual Conference of Indian Society of Critical Care and Disaster Medicine, AIIMS, Dec. 2004.
- 1st to 15th Annual Micro-neurosurgery Workshop; AIIMS, Delhi - Feb. 1999 to 2013.
- 3rd National Conference of Gamma Knife Radiosurgery on 12thFebruary, 2012 at Department of Neurosurgery, AIIMS.
- 61st Annual National Conference of Neurological Society of India and 1st Indo German Neurosurgical Society Friendship meeting at Gurgaon from 19th 22nd December, 2012
- Annual Conference of the Indian Society for Pediatric Neurosurgery (Ind ISPN) and International Society for Pediatric Neurosurgery (ISPN) 1st to 3rd November, 2012.
- Chairperson in various conferences of Neurological Society of India, Cereberovascular Society of India and Skull Base Surgery Society of India.
Membership of National and International Scientific Societies
- N.A.M.S. - National Academy of Medical Sciences
- I.M.A. - Indian Medical Association
- D.M.A. - Delhi Medical Association
- N.S.I. - Neurological Society of India
- D.N.A. - Delhi Neurological Association
- N.E.S. - Neuro-otological and Equilibriometric Society of India
- S.B.S.S.I. - Skull Base Surgery Society of India
- I.E.A. - Indian Epilepsy Association
- I.S.P.N. - Indian Society of Pediatric Neurosurgery
- I.S.S.F.N. - Indian Society of Stereotactic and Functional Neurosurgery
- N.T.S.I. – Neurotrauma Society of India
- N.O.S.I. - Neuro-Oncology Society of India
- A.C.N.S. - Asian Conference of Neurological Surgeons
- A.S.S.F.C.N. - Asian Society of Stereotactic, Functional and Computer - aided Neurosurgery
- C.N.S. – Congress of Neurological Surgeons (U.S.A.)
- N.A.S.S. – North American Spine Society
- N.S.S.I. – Neurological Surgeons Society of India
Elected offices in Professional Societies
- Co-Chairman: Academic Committee: Neurological Surgeons Society of India. NSSI
- Treasurer of S.B.S.S.I. - Skull Base Surgery Society of India 2009-2012
- Executive Member of the N.E.S.- Neuro-otological and Equilibriometric Society of India 2001/2002
- Executive Member of S.B.S.S.I.- Skull Base Surgery Society of India 2006-2009
- Executive Member of NSSI - Neurological Surgeons Society of India.
Memberships of editorial boards of journals
Member of the Editorial Board of
- International Journal of Neurology and Neurosurgery
- Journal of Craniovertebral Junction Surgery
- Indian Journal of Neurosurgery
Reviewer of articles for various national and international journals:
- National:Neurology India,
- Indian Journal of Paediatrics,
- Indian Journal of Medical Research,
- Indian Journal of Neurosurgery.
- International: Clinical Neurology and Neurosurgery,
- ActaNeurochirurjica.
Development of Specialty of Neurosurgery
Neurosurgery Skills Training Facility and Experimental Laboratory
The Department of Neurosurgery at the All India Institute of Medical Sciences, New Delhi started the “Experimental Microneurosurgery Laboratory” in 1971 through the efforts of Prof. P.N. Tandon and Prof. A.K. Banerji (Emeritus Professors, Department of Neurosurgery).
The training laboratory was expanded and renovated into a full fledged training facility named as Neurosurgery Skills Training Facility and Experimental Laboratory with the support of Department of Science and Technology (DST), Ministry of Science and Technology, Govt. of India, Department of Biotechnology (DBT) Indo-German Collaboration, Ministry of Science and Technology, Govt. of India, and Department of Health Research (DHR-ICMR), Ministry of Health and Family Welfare, Govt. of India for hands on skills training of M.Ch and DNB neurosurgery residents and trained /trainee Neurosurgeons from India and abroad.
The Neurosurgery Skills Training Facility and Experimental Laboratory is equipped with the state-of-the-art equipment, which simulates a modern Neurosurgery Operation Room environment. The training imparted is aimed at development of Neurosurgical skills and techniques.
The training imparted in the form of quarterly workshops, short term training programs and daily skills training sessions is focused on formulation of a new curriculum of neurosurgical skills development and imparting hands-on practice on synthetic/semi synthetic models, live anesthetized animals and cadaver parts using highly advanced equipment and technology creating a neurosurgical operation room environment.
http://aiimsnets.org/workshops.asp
Neurosurgery Education and Training School (NETS)Website
Neurosurgery Animation, Graphics and Video Editing Laboratory
Tele-education Platform
TEACHING EXPERIENCE
- Postgraduate and MCh trainee teaching sessions (AIIMS): moderator and supervisor in weekly case presentations, journal clubs, mortality and morbidity meetings.
- Interdepartmental meetings (AIIMS): weekly Neuro-radiology and Neuropathology meetings.
- Undergraduate teaching (AIIMS): integrated seminars and clinical case discussions.
- Nursing staff teaching (AIIMS)
- Neuro-technology teaching: IIT-Delhi
Invited speaker in numerous Continuing Medical Education (CME) programs, seminars, workshops and conferences.
Awards
- Merit Scholarship & Scholar Badge: Delhi Public School, R.K. Puram, New Delhi
- MBBS Gold Medalist: Final M.B.B.S. University College of Medical Sciences, New Delhi.
- North American Spine Society and The Spine Journal Outstanding Paper Award: North American Spine Society and The Spine Journal (Montreal)
- Best NSI Poster Award: Neurological Society of India (Cochin)
- Best ISPN Paper Award: Indian Society of Pediatric Neurosurgery (Lucknow)
- International Society of Pediatric Neurosurgery Scholarship: International Society of Pediatric Neurosurgery Scholarship (Monaco)
- Awards to Students for Research Work carried out under my guidance: National = 11, International= 1
Awards to Students for Research Work carried out under guidance :
- Payal Jotwani, received Best Paper Award: Computerized Evaluation Vs. Apprenticeship Method-based Evaluation: Effectualness of Micro-suturing Neurosurgery Skills Training in the 15th Annual Conference of Delhi Neurological Association from 16th to 17th February, at India Habitat Centre, New Delhi (DNACON 2013) ,Payal Jotwani, Ashish Suri, Prem Kalra*, Sanjiva Prasad*, Subhashis Banerjee*, Subodh Kumar*, Kollin Paul*, Sumit Bansal, Anand VK. (Department of Neurosurgery, AIIMS, and Department of Computer Science and Engineering, IIT*, Delhi)
- Dr. Siddhartha S.Sahoo received Best Neurosurgery Paper Award for the paper “ Outcome of revascularization in Moyamoya disease: Evaluation of new angiographic scoring system”: Dr.Siddhartha S Sahoo, Ashish Suri, S.Leve Joseph Devarajan, Sumit Bansal, B.S.Sharma, N.K.Mishra at the 61st Annual National Conference of Neurological Society of India and 1st Indo German Neurosurgical Society Friendship meeting at Gurgaon from 19th 22nd December, 2012
- Dr.Aanchal Kakkar received Best Neuro-oncology Award for the paper “Meningeal hemangiopericytoma- a clinicopathological immunohistochemical and molecular genetic study, with emphasis on MGMT (06-Methylguanine-DNA methyltransferase ) promoter methylation status” : Dr.Aanchal Kakkar, Prerana Jha, Supriyo Mallick, Nikhil Joshi, Nishant Goyal, Vaishali Suri, M.C.Sharma, Ashish Suriat the 61st Annual National Conference of Neurological Society of India and 1st Indo German Neurosurgical Society Friendship meeting at Gurgaon from 19th 22nd December, 2012
- Jotwani P, Suri A, Mahapatra AK, Prasad S, Banerji S, Kumar S, Kalra P, Bora S, Singh A.Awarded best paper at the 8th Biennial National Conference of Medical Informatics 3-5 Feb.2012 held at AIIMS by Indian Association of Medical Informatics (IAMI). Supplementing education and training in Neurosurgery: Web based education and Tele-education.
- Dr. Prerana Jha received First Prize for paper entitled “MGMT gene promoter methylation in gliomas” Prerana Jha, Vaishali Suri, Mehar Chand Sharma, Pankaj Pathak, Pankaj Jha, Arti Srivastava, Ashish Suri, Deepak Gupta, Kunzang Chosdol, Parthoprasad Chattopadhyay, Chitra Sarkar XIIth annual conference of DNA (DNACON- 2009 ), 6th and 7th Feb 2010 , Sir Ganga Ram Hospital, New Delhi.
- Dr.Shipra Agarwal received First Prize for poster entitled “Molecular profile of oligodendrogliomas in the young” Shipra Agarwal, Vaishali Suri, Prerana Jha, Pankaj Pathak, Arti Srivastava, Bhaskar Shukla, Ashish Suri, Manish Sharma, Mehar C. Sharma, ChitraSarkar. XIIth annual conference of DNA (DNACON- 2009)), 6th and 7th Feb 2010 , Sir Ganga Ram Hospital, New Delhi.
- Dr.Nilesh Kurwale received Best Paper Award in Annual Meeting of Neurological Society of India, Lucknow 2009 for paper ‘Effect of bone marrow-derived mononuclear cells on nerve regeneration in the transection model of the rat sciatic nerve.’ NileshKurwale, Suri V, Suri A, Sarkar C, Mohanty S, Sharma MC, Yadav PK, Srivastava
- Dr.Amit Thapa received Best Paper Award in DNACON 2009 (XI Annual conference of Delhi Neurological Association). 7th February 2009 for paper ‘Intraoperative pulse and blood pressure recordings from neurosurgeons during aneurysm clipping - navigating the frontiers of human cardiovascular performance’. AmitThapa, Manish S Sharma, Sharat P Chandra, A Suri, M Singh, V K Bahl, B S Sharma.
- Dr. Shipra Agarwal received Second Best Paper Award in DNACON 2009 (XI Annual conference of Delhi Neurological Association). 7th February 2009 for paper ‘Assessment of 1p19q deletion status by interphase fluorescence in-situ hybridization assay and co-relation with p 53 and EGFR expression: a comparative study in oligodendroglial and mixed oligoastrocytic and astrocytic tumors’. ShipraAgarwal, B Shukla, V Suri, P Phatak, MC Sharma, D Gupta, A Suri, BS Sharma, A Haldar, ChitraSarkar
- Dr. Shashank Ramdurg received Best Paper Award in Annual Meeting of Neurological Society of India, Pune 2008 for paper ‘Magnetic resonance imaging evaluation of subarachnoid hemorrhage in rats and the effects of intra-cisternal injection papavarine in the management of cerebral vasospasm- an experimental study”.ShashankRamdurg, A Suri, B S Sharma, NR Jaganathan.
- Dr. Sachin Anil Borkar received Indian Society of Pediatric Neurosurgery Traveling Fellowship for resident for 2008 and Second Best Paper Award in Neuropedicon-2008, 19th Annual Conference of Indian Society of Pediatric Neurosurgery, 7th-9th November, 2008, Coimbatore, India for paper “Pediatric glioblastomas: A clinico-pathological study of 45 cases at a tertiary care centre”. Sachin Anil Borkar, Ashish Suri, Prasenjit Das, Vaishali Suri, ChitraSarkar, Bhavani Shankar Sharma.
- Dr Anil Kumar Garg received International Society of Pediatric Neurosurgery Traveling Fellowship for resident for 2008 and Best Paper Award in International Society of Pediatric Neurosurgery Conference, Cape town, South Africa, 12-16th October, 2008 for paper “Changes in cerebral perfusion, hormone profile and CSF flow study following Endoscopic Third Ventriculostomy (ETV) for Hydrocephalus : A Prospective Study. Anil Kumar Garg, A Suri, BS Sharma, CS Bal
- Dr. Vaishali Suri won the Herbert Krause Gold Medal for the paper entitled “Pediatric glioblastomas, a histopathological and molecular genetic study” at the 56th Annual conference of Neurological Society of India, Agra, December 2007
- Dr. Shashank Ramdurg received Best Paper Award in Annual Meeting of Indian Society of Pediatric Neurosurgery at Chandigarh 2007 for paper “Infant mortality in neurosurgery: Need for raising a specialized cadre of neurointensivist ?” Shashank Ramdurg, A Suri, MM Singh, B S Sharma
- Dr Ashish Tandon received Best Poster Award for the poster entitled “Pituitary in head injuries”. In: Annual Conference of Neuro-Trauma, Pune, 2003.
Research Fields:
Innovation based research and development.
- Hospital of Barmherzige Brüder Trier, Trier, University of Mainz, Germany: Prof. Martin Bettag. Research & development of formulation of neurosurgery skills training curriculum.
- Department of Computer Science and Engineering, IIT-Delhi: Prof. Sanjiva Prasad, Prof. Prem Kalra, Prof. Subodh Kumar, Prof. Subhashish Banerji, Prof. Kollin Paul. Research & development: Virtual training platform: web-based, Real-time evaluation and assessment system of neurosurgery skills training, 3-D animation and graphics based E-learning modules, Virtual reality simulation.
- Department of Bio-Medical Engineering, IIT-Delhi: Prof. Sneh Anand. Research & development of Low cost versatile Neurosurgery instruments
Research in neurosurgery skills training.
- Research & development of formulation of neurosurgery hands-on skills training modules: In collaboration with Departments of Anatomy, Forensic Medicine and Central Animal Facility AIIMS.
- Research & development of formulation of virtual reality training platform: Web-based & E- Learning modules: In collaboration with IIT Delhi.
Laboratory based neurosurgery focused research.
- Cerebrovascular Research
- Stem Cell Research
Clinical research
Research Projects from Recognized National &International Agencies:
Completed Projects as Chief Investigator:
ANTISENSE PHARMA Gmb Josef-Engert-StraBe9D-93053 Regensburg Germany
A multi-national, multi-center, open-label, active-controlled, randomized parallel-group dose-finding study to evaluate the efficacy and safety of two doses of AP 12009 in adult patients with recurrent high-grade glioma, administered intratumorally as continuous high-flow microperfusion over a 7-day period every other week.
International Society of Pediatric Neurosurgery, (ISPN), International Study Group on Neuro-endoscopy, (ISGNE).
The International Infant Hydrocephalus Study (IIHS) is an international multi-center, prospective, controlled, randomized study of the treatment of newly diagnosed obstructive hydrocephalus in infants below 2 years of age.
Dept. of Science and Technology: FIST (DST-FIST), Ministry of Science and Technology, Govt. of India.
FIST sponsored AIIMS Neurosurgery Skills Training Facility and Experimental Laboratory (Cadaver Dissection Facility)
Department of Biotechnology (DBT), Ministry of Science and Technology, Govt of India.
Collaborative Indo-German Program for Bilateral Workshops, Seminars and Tele-education in Training Microsurgical and Endoscopic Techniques in Neurosurgery
Ongoing Projects as Chief Investigator:
Indian Council of Medical Research (ICMR), MinistryofHealth& Family Welfare, Govt. of India, AIIMS+ CSE- IIT-D
Evaluation of development of neurosurgery skills by hands - on skills training and interactive virtual training modules (web based, tele-education and real time simulation).
Department of Health and Research (DHR), Indian Council of Medical Research, MinistryofHealth& Family Welfare, Govt of India, AIIMS+ CSE- IIT-D
Expansion of DST + DBT Sponsored Neurosurgery Skills Training Facility and Development of Stereoscopic (3 Dimensional - 3D) Virtual Training Modules for Neurosurgery Skills Training
Department of Science and Technology - Instrumentation Development Program (DST- IDP), India. AIIMS+ BME- IIT-D: Development of Low-Cost Versatile Neurosurgery Equipment System for Neurosurgery
Dept. of Science and Technology: (DST-FIST Level II), Ministry of Science and Technology, Govt. of India. DST- for Neurosurgery Skills Training Facility (Cadaver Dissection Stations) and 3D Surgical Endoscopic and 3D Microscopic Integrated Digital Neurosurgery OR’s and Central Repository Server for Archival , Streaming and Teleconferencing.
Research projects as Co-investigator:
Codman (J & J)
A Registry for Comparing Catheter-Related Infection Among various Shunt-systems in the Treatment of Hydrocephalus
Indian Council of Medical Research (ICMR)MinistryofHealth& Family Welfare, Govt of India.
Study of the role of bone marrow derived mononuclear cells in peripheral nerve repair of adult rats.
Actelion Pharmaceuticals Ltd.Gewerbestrasse 16, CH-4123 Allschwil, Switzerland.
A Prospective, Multi-centre, double-blind, randomized, placebo-controlled,parallel-group study to assess the efficacy and safety of clazosentan in reducing vasospasm-related morbidity and all cause mortality in adult patients with aneurismal subarachnoid hemorrhage treated by surgical clipping.
London School of Hygiene and Tropical Medicine, London, UK.
CRASH-2 (Project NI-774) Clinical Randomization of Antifibrinolytic (Tranaexemic acid) in trauma pts with or at risk of Significant Hemorrhage (death / tranfusion requirement)
Peregrine Pharmaceuticals,Inc.14272 Franklin Avenue Suite100, Tustin , CA 92780-7017, 714-508-6000.
Open label, dose confirmation study of Interstial I131-ch TNTA/B MAb (COTARAR ) for the treatment of Recurrent GlioblastomaMultiforme (GBM) at first relapse.
Department of Biotechnology (DBT), Ministry of Science and Technology, Govt of India.
Hypoxia and p53-HIC1 axis in stemness of glial tumors and cell lines
Indian Council of Medical Research (ICMR)MinistryofHealth& Family Welfare, Govt of India.
Glioblastomas in children and adults: A comparative study with special reference to molecular pathways and MGMT methylation status.
ANTISENSE PHARMA Gmb Josef-Engert-StraBe9D-93053 Regensburg Germany
Efficacy and Safety of AP 12009 in Adult Patients with Recurrent or Refractory Anaplastic Astrocytoma (WHO grade III) as Compared to Standard Treatment with Temozolomide or BCNU: A Randomized, Actively Controlled, Open Label Clinical Phase III Study.
Ministry of Communication and Information Technology, Department of Electronics and Information Technology.
Foundation of Trusted and Scalable: Last Mile Healthcare, Indo-US joint R & D PROJECT BY IIT-Delhi, All India Institute of Medical Sciences (AIIMS –Delhi) C-DAC-Chennai, Dartmouth College & Rice University, USA.
Research Guidance:
Number of scholars who have been awarded M.Ch. / M.D./Ph.D degrees under supervision as guide \ co-guide:
| Awarded | Under Submission |
|---|---|
M.Ch.18 (Neurosurgery) | 2 |
M.S. 2 (ENT) | |
M.D. 2 (Anatomy) |
1 |
Ph.D. (Neuropathology) (Neurochemistry) (Biochemistry) (Microbiology) |
1 1 1 2 |
| PGDHHM 1 |
TOTAL NO. OF PUBLICATIONS
| Published | Under Publication | 1st /Comm. Author | |
1. Research Papers (a) Indexed Journals (b) Non-Indexed Journals | 114 112 2 | 12 | 76 74 2 |
2. Books (a) Text Books (b) Edited Books (c) Educational Books (d) E-Books | 140 seminars 20 operation videos 16 modules | 3D, animation and graphics modules | |
| 3. Chapter in Books | 9 | 2 | 9 |
4. Abstracts (a) Indexed Journals (b) Non-Indexed Journals | 72 20 52 |
Indexed Papers: 2005 to 2012 October
- Rathore YS, Chandra PS, Kumar R, Singh M, Sharma MS, Suri A, Mishra NK, Gaikwad S, Garg A, Sharma BS, Mahapatra AK. Monitored gradual occlusion of the internal carotid artery followed by ligation for giant internal carotid artery aneuryss.Neurol India. 2012;60 (2):174-9.
- Kurwale NS, Ahmad F, Suri A, Kale SS, Sharma BS, Mahapatra AK, Suri V, Sharma MC. Post operative pituitary apoplexy: preoperative considerations toward preventing nightmare.Br J Neurosurg. 2012; 26(1):59-63.
- Jain V, Rath GP, Dash HH, Bithal PK, Chouhan RS, Suri A Stellate ganglion block for treatment of cerebral vasospasm in patients with aneurysmal subarachnoid hemorrhage - A preliminary study.JAnaesthesiolClinPharmacol. 2011;27(4):516-21.
- Jha P, Suri V, Singh G, Jha P, Purkait S, Pathak P, Sharma V, Sharma MC, Suri A, Gupta D, Mahapatra AK, Sarkar C. Characterization of molecular genetic alterations in GBMs highlights a distinctive molecular profile in young adults.DiagnMolPathol. 2011;20 (4):225-32.
- Khandelwal D, Khadgawat R, Mukund A, Suri A. Acromegaly with no pituitary adenoma and no evidence of ectopic source. Indian J EndocrinolMetab. 2011;15Suppl 3:S250-2.
- Ammini AC, Bhattacharya S, Sahoo JP, Philip J, Tandon N, Goswami R, Jyotsna VJ, Khadgawat R, Chumber S, Seth A, Karak AK, Sharma BS, Chandra PS, Suri A, Sharma MS, Kale SS, Singh M.Cushing's disease: results of treatment and factors affecting outcome.Hormones (Athens). 2011;10(3):222-9.
- Jha P, Suri V, Sharma V, Singh G, Sharma MC, Pathak P, Chosdol K, Jha P, Suri A, Mahapatra AK, Kale SS, Sarkar C.IDH1 mutations in gliomas: first series from a tertiary care centre in India with comprehensive review of literature.ExpMolPathol. 2011;91(1):385-93. Epub 2011- 3. Review.
- Kurwale NS, Suri V, Suri A, Sarkar C, Gupta DK, Sharma BS, Mahapatra AK. Predictive factors for early symptomatic recurrence in pilocytic astrocytoma: does angiogenesis have a role to play? J ClinNeurosci. 2011;18 (4):472-7.
- Lakshmi Prasad G, Ramdurg SR, Suri A, Mahapatra AK. A rare association of meningioma with intratumoral bleed and acute subdural hematoma. Neurol India.2010; 58(6):977-8.
- Jha P, Suri V, Jain A, Sharma MC, Pathak P, Jha P, Srivastava A, Suri A, Gupta D, Chosdol K, ChattopadhyayP,Sarkar C. O6-methylguanine DNA ethyltransferase gene promoter methylation status in gliomas and its correlation with other molecular alterations: first Indian report with review of challenges for use in customized treatment. Neurosurgery. 2010;67(6):1681-91.
- Bogdahn U, Hau P, Stockhammer G, Venkataramana NK, Mahapatra AK, Suri A,Balasubramaniam A, Nair S, Oliushine V, Parfenov V, Poverennova I, ZaaroorM,Jachimczak P, Ludwig S, Schmaus S, Heinrichs H, Schlingensiepen KH; TrabedersenGlioma Study Group. Targeted therapy for high-grade glioma with the TGF-B2 inhibitor trabedersen: results of a randomized and controlled phase IIb study. Neuro Oncol. 2011;13(1):132-42.
- Das P, Puri T, Jha P, Pathak P, Joshi N, Suri V, Sharma MC, Sharma BS, Mahapatra AK, Suri A, Sarkar C. A clinicopathological and molecular analysis of glioblastomamultiforme with long-term survival. J ClinNeurosci. 2011;18(1):66-70.
- Kumar A, Kasliwal MK, Suri A, Sharma BS. Spontaneous asymptomatic rupture of cystic craniopharyngioma in a child: case report and review of the literature. J Child Neurol. 2010; 25(12):1555-8.
- Mishra S, Chandra PS, Suri A, Rajender K, Sharma BS, Mahapatra AK. Endoscopic management of third ventricular colloid cysts: eight years' institutional experience and description of a new technique. Neurol India. 2010;58(3):412-7.
- Ramdurg SR, Suri A, Gupta D, Mewar S, Sharma U, Jagannathan NR, Sharma BS. Magnetic resonance imaging evaluation of subarachnoid hemorrhage in rats and the effects of intracisternal injection of papaverine and nitroglycerine in the management of cerebral vasospasm. Neurol India. 2010;58(3):377-83.
- Ramdurg SR, Gupta DK, Suri A, Sharma BS, Mahapatra AK. Calvarial tuberculosis: Uncommon manifestation of common disease--a series of 21 cases. Br J Neurosurg.2010;24(5):572-7.
- Kasliwal MK, Basheer N, Suri A. Pituitary hormonal loss and recovery after transsphenoidal adenoma removal. Neurosurgery. 2010;67(1):221.
- Sharma MS, Thapa A, Chandra SP, Suri A, Singh M, Bahl VK, Sharma BS. Intraoperative pulse and blood pressure recordings of neurosurgeons: a pilot study of cardiovascular performance. Neurosurgery. 2010;66(5):893-9; discussion 899.
- Jha P, Agarwal S, Pathak P, Srivastava A, Suri V, Sharma MC, Chosdol K, Srivastava T, Gupta D, Gupta A, Suri A, Sarkar C. Heterozygosity status of 1p and19q and its correlation with p53 protein expression and EGFR amplification in patients with astrocytic tumors: novel series from India. Cancer Genet Cytogenet. 2010; 15;198 (2):126-34.
- Kumar A, Kasliwal MK, Suri A, Sharma BS. Spontaneous Asymptomatic Rupture of Cystic Craniopharyngioma in a Child: Case Report and Review of the Literature. J Child Neurol. 2010 Jul 23.
- Mishra S, Chandra PS, Suri A, Rajender K, Sharma BS, Mahapatra AK. Endoscopic management of third ventricular colloid cysts: Eight years' institutional experience and description of a new technique. Neurol India. 2010 May-Jun;58(3):412-7.
- Ramdurg SR, Suri A, Gupta D, Mewar S, Sharma U, Jagannathan NR, Sharma BS. Magnetic resonance imaging evaluation of subarachnoid hemorrhage in rats and the effects of intracisternal injection of papaverine and nitroglycerine in the management of cerebral vasospasm. Neurol India. 2010 May-Jun;58(3):377-83.
- Ramdurg SR, Gupta DK, Suri A, Sharma BS, Mahapatra AK. Calvarial tuberculosis: Uncommon manifestation of common disease - a series of 21 cases. Br J Neurosurg. 2010 Jul 15.
- Kasliwal MK, Basheer N, Suri A. Pituitary hormonal loss and recovery after transsphenoidal adenoma removal. Neurosurgery. 2010 Jul;67(1):221; author reply 221.
- Sharma MS, Thapa A, Chandra SP, Suri A, Singh M, Bahl VK, Sharma BS. Intraoperative pulse and blood pressure recordings of neurosurgeons: a pilot study of cardiovascular performance. Neurosurgery. 2010 May;66 (5):893-9; discussion 899.
- Jha P, Agarwal S, Pathak P, Srivastava A, Suri V, Sharma MC, Chosdol K, Srivastava T, Gupta D, Gupta A, Suri A, Sarkar C. Heterozygosity status of 1p and 19q and its correlation with p53 protein expression and EGFR amplification in patients with astrocytic tumors: novel series from India. Cancer Genet Cytogenet. 2010 Apr 15;198(2):126-34.
- Dagar A, Kasliwal MK, Suri A, Kumar S, Garg A, Sharma BS. A rare case of metachronous double spinal duralarteriovenous fistula. Neurol India. 2010 Jan-Feb;58(1):154-5.
- Yerramneni VK, Chandra PS, Kasliwal MK, Sinha S, Suri A, Gupta A, Sharma BS. Recovery of oculomotor nerve palsy following surgical clipping of posterior communicating artery aneurysms. Neurol India. 2010 Jan-Feb;58(1):103-5.
- Garg AK, Suri A, Sharma BS. Ten-year experience of 44 patients with moyamoya disease from a single institution. J ClinNeurosci. 2010 Apr;17(4):460-3. Epub2010 Feb 26.
- Basheer N, Kasliwal MK, Suri A, Sharma MC, Arora A, Sharma BS. Lateral extradural, supratentorialneurentericcyst. J Clin Neurosci. 2010 May;17(5):639-41. Epub 2010 Feb 25.
- Thapa A, Chandra PS, Sinha S, Gupta A, Singh M, Suri A, Sharma BS. Surgical interventions in intracranial arteriovenous malformations: indications and outcome analysis in a changing scenario. Neurol India. 2009 Nov-Dec;57(6):749-55.
- Kiran NA, Kasliwal MK, Suri A, Mahapatra AK. Giant posterior fossa arachnoid cyst associated with syringomyelia. ClinNeurolNeurosurg. 2010 Jun;112(5):454-5.Epub 2010 Feb 6.
- Kiran NA, Kasliwal MK, Suri A, Mahapatra AK. Intrathoracic migration of ventriculoperitoneal shunt. Indian J Pediatr. 2010 Mar;77(3):335.
- Chaturvedi D, Suri A, Kasliwal MK, Mahapatra AK, Mehta VS, Shridhar V, Garg A, Sarkar C, Dogra TD, Singh R. Factors affecting the development of hypothalamus and pituitary lesions in fatal closed head injury: a prospective study. J Trauma. 2010 Aug;69(2):290-3.
- Sharma BS, Kasliwal MK, Suri A, Sarat Chandra P, Gupta A, Mehta V.S. Outcome following surgery for ophthalmic segment aneurysms. J ClinNeurosci. 2010 Jan;17(1):38-42. Epub 2009 Dec 14.
- Kasliwal MK, Suri A. Insular gliomas and lenticulostriate artery position. J Neurosurg. 2009 Dec;111(6):1294; author reply 1294-5.
- Sharma S, Kalra V, Garg A, Suri V, Suri A. Gliomatosis cerebri. Indian J Pediatr. 2009 May;76(5):553-4. Epub 2009 Apr 23.
- Shukla B, Agarwal S, Suri V, Pathak P, Sharma MC, Gupta D, Sharma BS, Suri A, Halder A, Sarkar C. Assessment of 1p/19q status by fluorescence in situ hybridization assay: A comparative study in oligodendroglial, mixed oligoastrocytic and astrocytic tumors. Neurol India. 2009 Sep-Oct;57(5):559-66.
- Basheer N, Kasliwal MK, Suri A. Posterior communicating artery aneurysm associated with duplicated posterior communicating artery and bilateral fetal posterior cerebral arteries. Neurol India. 2009 Jul-Aug;57(4):514-5.
- Tandon A, Suri A, Kasliwal MK, Mahapatra AK, Mehta VS, Garg A, Sarkar C, Dogra TD, Pandey RM. Assessment of endocrine abnormalities in severe traumatic brain injury: a prospective study. ActaNeurochir (Wien). 2009 Nov;151(11):1411- 7.
- Goel RK, Suri V, Suri A, Sarkar C, Mohanty S, Sharma MC, Yadav PK, Srivastava Effect of bone marrow-derived mononuclear cells on nerve regeneration in the transection model of the rat sciatic nerve. J ClinNeurosci. 2009 Sep;16(9):1211-7. Epub 2009 Jul 10.
- Sharma MS, Vohra A, Thomas P, Kapil A, Suri A, Chandra PS, Kale SS, Mahapatra AK, Sharma B.S. Effect of risk-stratified, protocol-based perioperative chemoprophylaxis on nosocomial infection rates in a series of 31 927 consecutive neurosurgical procedures (1994-2006). Neurosurgery. 2009 Jun; 64(6):1123-30; discussion 1130-1.
- Faiz Uddin Ahmad, Ashish Suri, Ajay Garg, Ashok Kumar Mahapatra, Veer Singh Mehta. Post traumatic bilateral facial palsy causing severe psychosocial impairment. Pan Arabian Journal Of Neurosurgery 2009 April; 13(1): 125-127.
- Borkar SA, Kasliwal MK, Suri A, Sharma BS. Cervical Hemangioblastoma with holocord syrinx. Surg Neurol. 2009 Mar 27. [Epub ahead of print]
- Garg A, Suri A, Chandra PS, Kumar R, Sharma BS, Mahapatra AK. Endoscopic third ventriculostomy: 5 years' experience at the All India Institute of Medical Sciences. Pediatr Neurosurg. 2009;45(1):1-5. Epub 2009 Feb 17.
- Kalra V, Mishra D, Suri A, Seth R, Garg A. Intraventricular neurocysticercosis. Indian J Pediatr. 2009 Feb 10. [Epub ahead of print]
- Garg AK, Suri A, Sharma BS, Shamim SA, Bal CS. Changes in cerebral perfusion hormone profile and cerebrospinal fluid flow across the third ventriculostomy after endoscopic third ventriculostomy in patients with aqueductal stenosis: a prospective study. Clinical article. J Neurosurg Pediatr. 2009 Jan;3(1):29-36.
- Ramdurg SR, Gupta DK, Suri A, Sharma BS, Mahapatra AK. Spinal intramedullary tuberculosis: a series of 15 cases. Clin Neurol Neurosurg. 2009 Feb;111(2):115-8. Epub 2008 Dec 5.
- Suri V, Das P, Jain A, Sharma MC, Borkar SA, Suri A, Gupta D, Sarkar C. Pediatric glioblastomas: A histopathological and molecular genetic study. Neuro Oncol. 2008 Dec 9. [Epub ahead of print]
- Kasliwal MK, Suri A, Rishi A, Suri V, Sharma BS, Sarkar C. Symptomatic bilateral cerebellar mass lesions: an unusual presentation of intracranial xanthogranuloma. J Clin Neurosci. 2008 Dec;15(12):1401-4. Epub 2008 Oct 25.
- Kurwale NS, Ahmad FU, Satyarthi G, Suri A, Mahapatra AK. Can radiation induce pituitary tumors? Giant prolactinoma after radiation exposure. J Clin Neurosci.2008 Nov;15(11):1287-8. Epub 2008 Oct 1.
- Goel RK, Ahmad FU, Vellimana AK, Suri A, Chandra PS, Kumar R, Sharma BS, Mahapatra AK. Endoscopic management of intraventricular neurocysticercosis. J Clin Neurosci. 2008 Oct;15(10):1096-101. Epub 2008 Jul 23.
- Kasliwal MK, Suri A, Sai Kiran NA, Sharma BS. Spontaneous thrombosis of giant cavernous internal carotid artery aneurysm in a neonate. Case report and review of the literature. Pediatr Neurosurg. 2008;44(4):329-32. Epub 2008 May 27. Review.
- Sharma BS, Gupta A, Ahmad FU, Suri A, Mehta V.S. Surgical management of giant intracranial aneurysms. Clin Neurol Neurosurg. 2008 Jul;110(7):674-81. Epub 2008 May 19.
- Suri V, Sharma MC, Suri A, Karak AK, Garg A, Sarkar C, Jain D. Myelolipomatous change in an interhemispheric lipoma associated with corpus callosum agenesis: case report. Neurosurgery. 2008 Mar;62(3):E745; discussion E745.]
- Suri A, Goel RK, Ahmad FU, Vellimana AK, Sharma BS, Mahapatra AK.Transventricular, transaqueductal scope-in-scope endoscopic excision of fourth ventricular neurocysticercosis: a series of 13 cases and a review. J Neurosurg Pediatr. 2008 Jan; 1(1):35-9. Review.
- Kasliwal MK, Suri A, Gupta DK, Suri V, Rishi A, Sharma BS. Sphenoid wing inflammatory pseudotumor mimicking a clinoidal meningioma: case report and review of the literature. Surg Neurol. 2008 Nov;70(5):509-13; discussion 513. Epub 2008 Jan 22. Review.
- Ajay Garg, Atin Kumar, Faiz Uddin Ahmad, Ashish Suri. Occipital condyle fracture with lower cranial nerve palsies in a patient with minor head injury. Pan Arabian Journal Of Neurosurgery2008 April; 12(1): 66-69.
- Suri A, Narang KS, Sharma BS, Mahapatra AK. Visual outcome after surgery in patients with suprasellar tumors and preoperative blindness. J Neurosurg. 2008 Jan;108(1):19-25.
- Kasliwal MK, Suri A, Sharma BS. Dandy Walker malformation associated with syringomyelia. Clin Neurol Neurosurg. 2008 Mar;110(3):317-9. Epub 2007 Dec 3.
- Kasliwal MK, Yerramneni VK, Sai Kiran NA, Suri A, Mahapatra AK, Sharma MC, Garg A. Giant sphenoethmoidal nasopaharyngeal schwannoma with anterior skull base extension managed by a total anterior transbasal approach. Neurol India. 2007 Oct-Dec;55(4):429-31.
- Kiran NA, Suri A, Kasliwal MK, Garg A, Ahmad FU, Mahapatra AK. Gross total excision of pediatric giant cystic craniopharyngioma with huge retroclival extension to the level of foramen magnum by anterior trans petrous approach: report of two cases and review of literature. Childs Nerv Syst. 2008 Mar;24(3):385-91. Epub 2007 Nov 23. Review.
- Suri A, Goel RK, Ahmad FU, Vellimana AK, Sharma BS, Mahapatra AK.Endoscopic excision of intraventricular neurocysticercosis in children: a series of six cases and review. Childs Nerv Syst. 2008 Feb;24(2):281-5. Epub 2007 Nov 10.
- Garg A, Agrawal D, Suri A, Mahapatra AK. Subdural empyema in a case of Gaucher disease: a rare presentation. Pediatr Neurosurg. 2007;43(6):531-2.
- Prabhakar H, Bithal PK, Suri A, Rath GP, Dash HH. Intracranial pressure changes during Valsalva manoeuvre in patients undergoing a neuroendoscopic procedure. Minim Invasive Neurosurg. 2007 Apr;50(2):98-101.
- Mridha AR, Sharma MC, Sarkar C, Suri V, Rishi A, Garg A, Suri A. Myxopapillary ependymoma of lumbosacral region with metastasis to both cerebellopontine angles: report of a rare case. Childs Nerv Syst. 2007 Oct;23(10):1209-13. Epub 2007 Jul 21.
- Dwarakanath S, Suri A, Sharma BS, Mahapatra AK. Neuronavigation in a developing country: A pilot study of efficacy and limitations in intracranial surgery. Neurol India. 2007 Apr-Jun;55(2):111-6.
- Mridha AR, Sharma MC, Sarkar C, Suri V, Garg A, Suri A. Primary liposarcoma of the orbit: a report of two cases. Can J Ophthalmol. 2007 Jun;42(3):481-3.
- Sai Kiran NA, Kasliwal MK, Suri A, Sharma BS, Suri V, Mridha AR, Sharma MC, Garg A. Eumycetoma presenting as a cerebellopontine angle mass lesion. Clin Neurol Neurosurg. 2007 Jul;109(6):516-9. Epub 2007 Apr 20.
- Prabhakar H, Rath GP, Bithal PK, Suri A, Dash H.H Variations in cerebral haemodynamics during irrigation phase in neuroendoscopic procedures. Anaesth Intensive Care. 2007 Apr;35(2):209-12. Erratum in: Anaesth Intensive Care. 2007 Jun;35(3):459.
- Garg A, Ahmad FU, Suri A, Mahapatra AK, Mehta VS, Atri S, Sharma MC, Garg A. Primary Ewing's sarcoma of the occipital bone presenting as hydrocephalus and blindness. Pediatr Neurosurg. 2007;43(2):170-3.
- Suri A, Ahmad FU, Mahapatra AK.Extradural transcavernous approach to cavernous sinus hemangiomas. Neurosurgery. 2007 Mar;60(3):483-8; discussion 488-9.
- Sharma BS, Sinha S, Mehta VS, Suri A, Gupta A, Mahapatra AK. Pediatric intracranial aneurysms-clinical characteristics and outcome of surgical treatment. Childs Nerv Syst. 2007 Mar;23(3):327-33. Epub 2006 Nov 21.
- Sharma BS, Sinha S, Suri A. Treatment of Giant Pituitary Adenomas. Neurosurgery Quarterly 2007 .17(2):120-127.
- Atri S, Sharma MC, Sarkar C, Garg A, Suri A. Papillary glioneuronal tumour: a report of a rare case and review of literature. Childs Nerv Syst. 2007 Mar;23(3):349-53. Epub 2006 Oct 13. Review.
- Rath GP, Mukta, Prabhakar H, Dash HH, Suri A. Haemodynamic changes after intracisternal papaverine instillation during intracranial aneurysmal surgery. Br J Anaesth. 2006 Dec;97(6):848-50. Epub 2006
- Sep 19.
- Dwarakanath S, Suri A, Sharma BS, Mehta VS. Intracranial hemangioblastomas: an institutional experience. Neurol India. 2006 Sep;54(3):276-8.
- Ahmad FU, Mahajan H, Mahapatra AK, Suri A. Mycotic aneurysm: an unusual cause of pyrexia of unknown origin in an immunodeficient infant. Pediatr Neurosurg. 2006;42(4):237-9.
- Gupta DK, Suri A, Mahapatra AK, Mehta VS, Garg A, Sarkar C, Ahmad FU. Intracranial Rosai-Dorfman disease in a child mimicking bilateral giant petroclival meningiomas: a case report and review of literature. Childs Nerv Syst. 2006 Sep;22(9):1194-200. Epub 2006 Mar 16. Review.
- Suri A, Ahmad FU, Mahapatra AK, Mehta VS, Sharma MC, Gupta V. Mediastinal extension of an intradural teratoma in a patient with split cord malformation: case report and review of literature. Childs Nerv Syst. 2006 Apr;22(4):444-9. Epub 2005 Oct 12. Review.
- Sharma A, Garg A, Mishra NK, Gaikwad SB, Sharma MC, Gupta V, Suri A. Primary Ewing's sarcoma of the sphenoid bone with unusual imaging features: a case report. Clin Neurol Neurosurg. 2005 Oct;107(6):528-31. Epub 2004 Dec 13.
- Sharma MS, Suri A, Shah T, Ralte A, Sarkar C, Gupta V, Mehta VS. Intraventricular glioneuronal hamartoma: histopathological correlation with magnetic resonance spectroscopy. J Neurooncol. 2005 Sep;74(3):325-8.
- Ahmad FU, Suri A, Mahapatra AK, Mehta VS, Garg A, Sharma MC, Sridhar E.Intraventricular rhabdoid tumor. Indian J Pediatr. 2005 Aug;72(8):693-6.
- Gupta DK, Suri A, Mahapatra AK, Mehta VS, Sarkar C, Kumar L. When an unusual lesion occurs in an odd place. Spine J. 2005 Jul-Aug;5(4):471-2.
- Ahmad FU, Suri A, Mahapatra AK.Fatal penetrating brainstem injury caused by bicycle brake handle. Pediatr Neurosurg. 2005 Jul-Aug;41(4):226-8.
- Sharma S, Sarkar C, Gaikwad S, Suri A, Sharma MC. Primary neurocytoma of the spinal cord: a case report and review of literature. J Neurooncol. 2005 Aug;74(1):47-52.
- Dwarakanath S, Suri A, Mahapatra AK, Mehta VS, Gaikwad S, Sarkar C. Endoscopic assisted excision of a retroclival arachnoid cyst presenting as hysterical breathlessness. Childs Nerv Syst. 2006 Apr;22(4):
- 424-7. Epub 2005 Jul 29.
Indexed Abstracts
- Suri A. Posterior Cavernous Anterior TranspetrosalPostero-medial Rhomboid (Dolenc-Kawase Rhomboid) Approach to Posterior Cavernous and Petroclival Lesions. Skull Base, Vol 22, Suppl 1., 2012, 18
- Suri A. Extradural Transcavernous Approach to Cavernous Sinus Hemangiomas. Skull Base, Vol 22, Suppl 1.,2012,20
- Ashish Suri, SumitBansal, Bhawani Sharma, Ashok K Mahapatra, Sharad S Kale, Sarat P Chandra, Manmohan Singh, Rajinder Kumar, Manish S Sharma Hypoglossal Schwannomas: Single Institutional Experience of 14 Cases. Skull Base, Vol 22, Suppl 1., 2012, 45
- Ashish Suri, SumitBansal, Ashok K Mahapatra, ManmohanSingh,Jugular Foramen Schwanomas : Single Institutional Experience of 28 cases. Skull Base, Vol 22, Suppl 1., 2012, 75
- Vaishali Suri, SawanKumar,LaxmiMohan,UtkarshBhagat, Ashish Suri, M.C. Sharma, Citra Sarkar, Evaluation of Molecular Alterations in PetroclivalMeningiomas and their correlation with extent of Tumor Resection, Skull Base, Vol 22, Suppl 1., 2012, 20
- Ashish Suri. Extradural Transcavernous Approach to Cavernous Sinus Hemangiomas Series of 10 Cases and Review; Skull Base/Volume 18, Supplement 1, 2008.
- Ashish Suri. Posterior Cavernous Anterior Transpetrosal Postero-medical Rhomboid (Dolenc-Kawase Rhomboid ) Approach tp Posterior Cavernous and Petroclival Lesions; Skull Base/Volume 18, Supplement 1, 2008.
- Vaishali Suri, Deepak Gupta, Ashish Suri, Chitra Sarkar, BS Sharma, A.K.Mahapatra.Petroclival Meningiomas: a clinico-pathological correlation; Skull Base/Volume 18, Supplement 1, 2008.
- Ashish Suri, Rohit. K Goyal, P.S.Chandra, R.Kumar, B.S Sharma.Endoscopic Treatment of Intracranial Lesions. Japanese Neuroendoscopy SL1-01, Supplement 1, 2008.
- Ashish Suri, Anil K Garg,P.S.Chandra,R.Kumar,B.S Sharma.Ideal treatment of Pediatric hydrocephalus : shunt v/s ETV. (Japanese Neuroendoscopy PD1-08, Supplement 1, 2008).
- A.Suri, P.S.Chandra, A.K.Mahapatra, V.S.Mehta; Endoscopic treatment of pediatric hydrocephalus; Child’s Nervous System 2003 (Aug.); 19(7-8): 617.
- A.Suri, A.Tandon, A.K.Mahapatra, V.S.Mehta; Pediatric orbital tumors; Child’s Nervous System 2003 (Aug.); 19(7-8): 625.
- P.S.Chandra, A.Suri, V.S.Mehta; Endoscopic excision of colloid cysts; Child’s Nervous System 2003 (Sept.); 19(9): 691.
- A.Suri, P.S.Chandra, A.K.Mahapatra, V.S.Mehta; Neuroendoscopic treatment of pediatric hydrocephalus: dilemmas and controversies; Child’s Nervous System 2003 (Sept.); 19(9): 687
- A.K.Mahapatra, A.Suri; Anteriorencephaloceles- a surgical correlation of 103 cases; Child’s Nervous System 2002 (Oct.); 18(9-10): 554.
- Suri A, Chabbra RPS, Mehta VS, Gaikwad S, Pandey RM. Effect of Intramedullary Signal Changes on the Surgical Outcome of Patients of Cervical Spondylotic Myelopathy. The Spine Journal. 2002; (2) 5S: 69S.
- Suri A, S.S.Kale, P.S.Chandra, Chabbra RPS, A.K.Mahapatra, Mehta VS. Developmental osseous craniovertebral junction anomalies: controversies and dilemmas. Neurosurgery. 2002; 51(2): 543.
- A.Suri , V.S. Mehta; factors affecting outcome after severe head injury: Neurology India; 1999 (Dec.) ; 47(Supple.1): 82.
- A.Suri , V.S. Mehta , C. Sarkar ; Microsurgical anastomosis of peripheral nerves: A comparison between microsurgical sutures and fibrin glue: Neurology India ; 1998 (Dec.) ; 46(Suppl. 1): 32.
- Suri A. , A.K. Mahapatra , P. Bithal ; Early and Late Seizures following posterior fossa surgery; Clinical Neurology and Neurosurgery ; 1997 (July); 99 (Suppl.1); P – 5 – 692
Chapters:
- Suri A, Mishra S, Garg A. Spinal Epidural and Intramedullary Abscess: Textbook of Neurosurgery P.N.Tandon and Ravi Ramamurthy 3rd Edition, Published by JAYPEE Publishers. Volume 2,Section 7, Infection, page no 718-722.
- Suri A, Borkar S, Mishra NK. Posterior Circulation Aneurysms: Textbook of Neurosurgery P.N.Tandon and Ravi Ramamurthy 3rd Edition, Published by JAYPEE Publishers. Volume 2,Section 8, Vascular Disorder, page no 996-1004.
- Suri A, Mishra S, Garg A. Other Intracranial Schwannoma: Textbook of Neurosurgery P.N.Tandon and Ravi Ramamurthy 3rd Edition, Published by JAYPEE Publishers. Volume 2,Section 12B, Cranial and Intermedullary Tumors, page no 1811-1815.
- A Suri, AK Garg, PS Chandra, R Kumar, BS Sharma, AK Mahapatra. Endoscopic Third Ventriculostomy in Infantile Hydrocephalus: Progress in Clinical Neurosciences 2007; 11: 579-595.
- A Garg, A Suri, S Gulati: CNS Tumors; Current Trend in Pediatrics, 2004; Vol 2: 382-403.
- Mehta V.S., Sharma B.S., Suri A, Gupta A., Misra N.K.: “Management of Giant Intracranial Aneurysms”: Progress in Clinical Neurosciences 2004: 168-180 ed. By. B.S. Sharma,U.K. Mishra(eds) New Delhi 2004
- V.S. Mehta, A.Suri; Posterior Circulation Aneurysms: In: Textbook of Operative Neurosurgery III Ed; B. Ramamurthy, P.N.Tandon 2002
- Suri A.,V.S. Mehta ,V.P.Singh, N.K.Mishra, H.H.Dash: Posterior Circulation Aneurysms : In : Progress in Clinical Neurosciences , 1999; 14: 127-150.
- Suri A., A.K. Mahapatra; Changing pattern of organisms in postoperative neurosurgical infections; Progress in Clinical Neurosciences 1996; 11: 365-369.

Dr.
P SARAT CHANDRAMCh
Male
Affiliation
Professor
Department of
Neurosurgery
Contact
Email :
saratpchandra@gmail.com
Brief Summary:
Dr P Sarat Chandra is currently a senior Professor, Dept of Neurosurgery at the reputed All India Institute of Medical Sciences (AIIMS), New Delhi for 22 years.
Initial Education: Dr Chandra has graduated his MBBS with honors and distinction in Physiology and Surgery and was the best outgoing student of his batch (Pfizer gold medalist). He completed his neurosurgical training from NIMHANS, Bangalore and then joined AIIMS as a faculty in 1998.
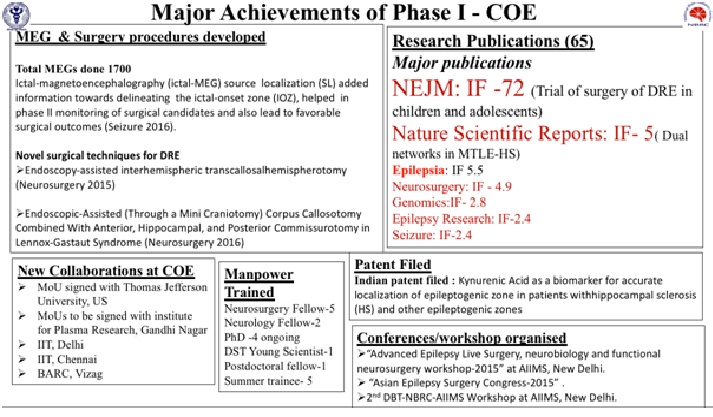
Publications: Dr Chandra over his course of 22 years operated over 25000 cases, 2000 epilepsy surgeries and published 492 papers (https://scholar.google.com/citations?user=C_fTZQsAAAAJ&hl=en), was awarded 14 extra mural major research grants and 9 patents.
Research and contributions: He has 3 major research projects (funded by Dept of Biotechnology, Ministry of Science and Technology and Principle Scientific Advisor’s Office to the Prime Minister), completed 14 extra-mural research projects,
He has trained over 35 residents and PhD’s. Also 9 fellows in epilepsy & epilepsy surgery from several parts of India and other countries (Indonesia, Nepal, Kenya). All fellows have successfully established their own epilepsy surgery programs in their respective centres.
He established the Centre of Excellence for Epilepsy and MEG resource facility, the first of its kind of facility in India with [1.]Advanced epilepsy surgery centre [2.]Advanced brain mapping and electrophysiological centre [3.]Advanced molecular/intra-cellular electrophysiology. The centre has its own research faculty, PhD students, technicians and fellows (again for first time in India) for seamless integration of clinical/ research work to study causes of drug-resistant epilepsy. Till date > 10 PhD’s passed out are in full-time research careers in epilepsy. His centre helped in raising awareness towards epilepsy research in India.The YouTube link shows a short summary movie about the COE and MEG resource facility and its achievements. https://youtu.be/EiXyk1HdA4E
Dr Chandra is also the lead Principle investigator for a prestigious project “Advanced research for epilepsy”, a multi institutional first of its kind of project funded by Office of Principle Scientific Advisor (PSA) to Govt. of India (Role of dysfunctional benzodiazepine binding site on GABAA receptor in benzodiazepine-resistance; mass spectrometric lipid profiles in FCD’s and molecular modelling/identification of novel drug targets).
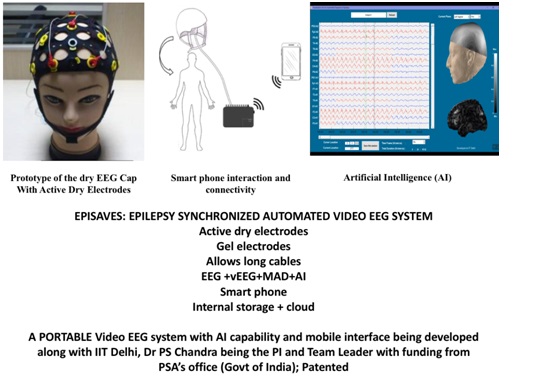
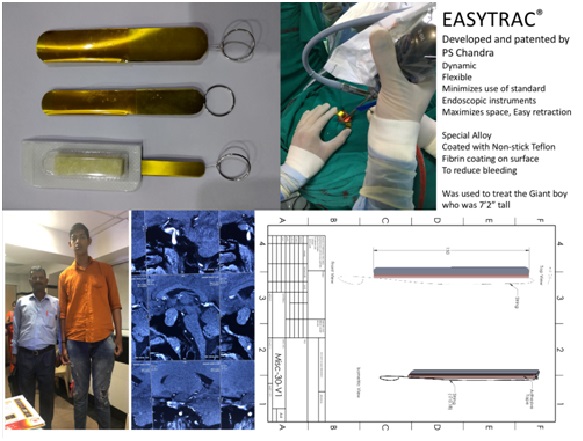
He has 9 patents, including 1 patent with USA and PCT (Paris Convention Treaty) International patent. He has developed new surgical techniques for the first time which have been validated and published. These include 1.] Endoscopic Hemispherotomy for epilepsy: a minimally invasive procedure, 2.] Robotic thermocoagulative hemispherotomy: a bloodless surgery 3.] Endoscopic corpus callosotomy for epilepsy: a minimally invasive procedure to treat severe drug resistant epilepsy 4.] Radiofrequency ablation disconnection of hypothalamic hamartoma using Robotic and O-arm guidance: a minimally invasive technique for these challenging lesions. 5.] Distraction, Compression, Extension and Reduction (DCER) for severe AAD and Basilar invagination in a single stage surgery.6.] Expandable tubular retractor for endoscopic pituitary surgery. 7.] Portable video EEG system with link to a mobile app and AI (along with IIT-D), called EPISAVES-see below.
His key areas of research include: Study of various bio-markers/receptors in abnormal epileptogenic areas (histone deacetylases alterations, altered kynurenine pathway metabolism, IDH-R132H-FAT1-ROS-HIF-1alfa signalling pathways, mTOR pathway in FCD’s, genome-wide DNA methylation and RNAseq analysis, GABA receptor mediated epileptogenicity, epigenetic regulations, endogenous activity of NMDA receptors, dual networks)
Some specific contributions for epilepsy:
Dr Chandra has organized several International meetings/teaching programs to enhance Epilepsy Surgery outreach along with several invited International faculty. Some include [1.] Annual COE EEG & epilepsy surgery Master Classes organized in various parts of India, 2012-2020 (8 years, AIIMS Rishikesh, AIIMS Raipur, BHU Varanasi, AIIMS Bhubaneswar, AIIMS Patna, & AIIMS Delhi) [2.] Epilepsy Schools at AIIMS Jodhpur (2019) [3.] Asian Epilepsy Surgery Congress, Udaipur, 2015 [4.] Organizer and faculty for Epilepsy Conclaves 2016-2018 [5.] Current trends in Epilepsy with host of International faculty 2006 [6.] ILAE & ASEPA workshop on epilepsy surgery, 2009 [7.] 1st Indo-German Neurosurgical meeting of Neurological Society of India Annual Congress (>4000 delegates).
He delivered Invited lectures (>100) in several International congresses. Some include ILAE (IEC, Vienna, 2018, AOEC (2016, 2007) , AESC (2020, Taiwan, online; 2019 Japan; 2018 Shanghai; 2016 Korea; 2015 Udaipur; 2012-2020) and ESTM (Gothenburg 2014, Prague 2016, Vienna 2018 and online in 2020), Japanese epilepsy society (2018,2017, 2016, 2008), CNS(Houston, 2018; Boston 2017); Annual Congress of Japanese Neurological surgeons (2017). His talks focus on developing strategies to make epilepsy surgery affordable and effective in developing countries especially based on this own experience of >2000 cases. He also advocates the need to amalgamate research with clinical work and the need to enhance epilepsy surgery outreach. He has described new techniques on epilepsy surgery: Endoscopic hemispherotomy/corpus callosotomy and Robotic thermo-coagulative hemispherotomy (ROTCH). The latter is a “bloodless” technique of hemispherotomy using thermo coagulation disconnection (https://www.youtube.com/watch?v=qRUfiPp5csU&t=3604s), now published in JNS Pediatrics.
He has performed demonstration surgeries in India and internationally, teaching epilepsy surgeries along with minimally invasive techniques (Mumbai, Surat, various AIIMS, Delhi, Jabalpur) and also in various countries (Kula Lumpur, Malaysia 2016, Indonesia 2013, 2015, 2017, 2018; Morocco 2015,2016, 2017, 2018; Kathmandu 2015, 2017, 2018). Most demonstrations also include endoscopic hemispherotomy and corpus callosotomy which has reduced morbidity and duration of hospital stay significantly.
He is on executive board of several International bodies [1.] Member, Epilepsy Surgery Task Force, ILAE (https://www.ilae.org/p-sarat-chandra) [2.] Member, Epilepsy Surgery, Developing World, ILAE (https://www.ilae.org/p-sarat-chandra) [3.] Co-Chair, Epilepsy Surgery section, AOEC, ILAE [4.] President Elect, Indian Epilepsy Society (IES), local chapter affiliated to ILAE [5.] Faculty 1000, ILAE [6.] Ex member, Paediatric Epilepsy Surgery Sub-commission, ILAE [7.] Ex-President, Asian Epilepsy Surgery Congress [8.] Ex board member of Indian Epilepsy Society [8.] Ex-Board member for Society for Brain mapping and therapeutics (SBMT).He has been on board the paediatric sub-commission to create the guidelines for paediatric epilepsy surgery. He has contributed towards Guidelines for epilepsy management in India (GEMIND), which is now online.
As a Co-Chair of Epilepsy Surgery of AOEC, he is conducting epilepsy-surgery sensitization classes for Nepal and Bhutan. He is developing an mobile app for collecting epilepsy surgery database from developing countries in Asia. The app is so designed to be intuitive, easy to use to allow easy entry of data. This would be the first of its kind for Asia and AOEC.
He was the main contributor for surgery for surgical arm for the first ever RCT for paediatric epilepsy surgery [Diwedi R et al; N Engl J Med 2017 Oct 26;377(17): 1639-1647; https://pubmed.ncbi.nlm.nih.gov/29069568/; Chandra PS et al; N Engl J Med 2018 Jan 25;378(4):399; https://pubmed.ncbi.nlm.nih.gov/29365299/]. The study demonstrated a 10 fold improvement of good outcome for surgery in Children vs medical treatment (77% vs 7%). It also demonstrated better cognitive outcomes for surgery in Children with drug resistant epilepsy as compared to medical therapy demonstrating the need for early surgery.
He contributed for HOPS (Hemispherectomy-Outcome-Prediction-Scale study, LANCET, https://papers.ssrn.com/sol3/papers.cfm?abstract_id=3514748). The study analysed 1237 hemispheric surgeries in paediatric patients, 31 centres, 12 countries to identify predictors of seizure freedom after surgery.
Epilepsy Self-help social groups: Co-founder of Ekatwam. This group is involved in providing free medicines and helping poor patients with the cost of epilepsy surgery. This group has now helped > 10,000 patients. (https://www.facebook.com/pages/category/Non-Governmental-Organization--NGO-/Ekatwam-Epilepsy-Delhi-243645915696765/).
Patents in Epilepsy:
- Kynurenic Acid as a biomarker for accurate localization of epileptogenic zone in patients with hippocampal sclerosis (HS) and other epileptogenic zones- Indian patent: 201711027150
- EPISAVES- Epilepsy Patient Integration of Synchronized Automated Video EEG System: A Portable, Automated, Video-EEG (with AI integration) and Smartphone Connectivity & Medicine Adherence System for seizure monitoring and comprehensive patient care. Patent: 201811033960 (grant from Office of PSA, Govt of India); Preliminary Study-Swami P, Chandra PS, Gandhi TK et al. Selection of optimum frequency bands for detection of epileptiform patterns. Healthc Technol Lett. 2019; https://pubmed.ncbi.nlm.nih.gov/31839968/ .
Specific contributions for Spine: Dr Chandra has been a pioneer from developing new techniques for cranio-vertebral junction especially for congenital
Others: He has been part of National program for development of a National program for epilepsy surgery collaborating with the Ministry of Health Government of India (Chandra PS et al. Epilepsy surgery: recommendations for India. Ann Indian Acad Neurol. 2010; https://pubmed.ncbi.nlm.nih.gov/20814490/).
Summarizing his primary area of focus has been Epilepsy, Epilepsy surgery and epilepsy networks where he has contributed significantly providing new surgical techniques, understanding mechanisms of epileptogenesis and epilepsy networks and also provided and created research and training facilities to take this further. He has also contributed in spine (cranio-vertebral junction and Vertebral body haemangiomas) by creating new surgical techniques, patenting new instruments and implants which have made the surgery easier, safer, and with less morbidity. He also has had significant experience in minimally invasive skull base surgery, robotic neurosurgery and cerebrovascular surgery. He also occupies leadership positions in several scientific societies and bodies.
Current Designation:
- Professor, Neurosurgery, All India Institute of Medical Sciences (AIIMS), New Delhi
- liI and Team Leader, Center of Excellence for Epilepsy and MEG facility (www.coeepilepsy.in)
Additional Designation Held:
- Fellow, UCLA, Los Angeles
- President Elect, Indian Epilepsy Society
- Past President, Asian Epilepsy Surgery Society.
- Committee member, Epilepsy Surgery Developing world and Epilepsy Surgery Task force, International League Against Epilepsy (ILAE)
- Editor Neurology India (estt 1953, Impact factor 2.1)
- Past Secretary, Skull Base Society of India (www.sbssi.org)
- President, Skull Base Society of India
- Secretary, Cerebro-vascular Society
- Faculty 1000, International League Against Epilepsy
- Alumini, San servolo summer school for epilepsy, Venice
- Penry fellow, Wakeforest University, North Carolina, USA
- Executive member and Hon’ble Treasurer, Neurological Society of India
- Past Executive member, Indian Epilepsy Society
Teaching Experience: 24 years, Surgical experience; over 25000 cases
Subspecialities:
- Epilepsy surgery:
- Personal experience of over 2000 cases
- Devised endoscopic techniques for hemispherotomy, corpus callosotomy and lobar disconnection, Robotic guided thermocoagulative hemispherotomy
- Started SEEG in India
- Director of Center of Excellence for Epilepsy (www.coeepilepsy.in)
- Spine:
- Craniovertebral junction and complex spine instrumentation especially for cervical spine
- Described a new technique for surgery called DCER which reduces operating time, morbidity by over 50%
- Minimally invasive spine surgery: endoscopic discectomy, percutaneous automated discectomy, percutaneous pedicle screw fixation.
- Neuroendoscopy and minimally invasive surgery
- Neuroendoscopy:
- Started neuroendoscopy in AIIMS in 1998
- Experience with over 1000 cases
- Has devised new techniques like endoscopic disconnective surgery for epilepsy & Endoscopic end endonasal trans-septal robotic guided surgery for pituitary tumors
- Others:
- Started robotic neurosurgery in AIIMS
- Cerebrovascular- specialized in minimally invasive eyebrow aneurysm surgery and clipping of complex aneurysms
- Tumors
- Skull Base Surgery- Petroclival tumors, Clival base tumours
Medical Schooling & Teaching experience and Medical education:
1985-1991 MBBS: Honours with gold medal in physiology, General Surgery. Best outgoing student of the batch, Pfizer gold medal as the best outgoing student. Jun 1991 – Jun 1998 Senior Resident and Pool officer (jr Lecturer)
National Institute of Mental Health and Neuro Sciences, Department of Neurosurgery
Bangalore, India
Jul 2005 – Aug 2006 Post Doc Fellow
University of California, Los Angeles, Department of Neurosurgery
Los Angeles, United States
Aug 1998 – 2003 Asst Professor
All India Institute of Medical Sciences, Department of Neurosurgery
New Delhi, India
2003-2008 Associate Professor
All India Institute of Medical Sciences, Department of Neurosurgery
New Delhi, India
2008-2011 Additional Professor
All India Institute of Medical Sciences, Department of Neurosurgery
New Delhi, India
2011-present Professor
All India Institute of Medical Sciences, Department of Neurosurgery
New Delhi, India
- Awards:
- Tadokaro award, ILAE (2006)
- Awarded the prestigious Sun Pharma award 2019 for best clinical researcher in India (https://www.sunpharmasciencefoundation.net/LatestWinnersResearchAwardmain.asp),
- AIIMS excellence award for best clinical researcher 2018
- Awarded the prestigious Fellowship of National Academy of Sciences (NASI), India, 2020, see page 364; (http://nasi.nic.in/Fellowship%20Nomination%20Book%202016/Biological_Sciences_Section_Book_II.pdf);
- Visiting Professor, International Neurosciences Institute (INI), Hannover, Germany
- Awarded the Annual Research Orator at the 3rd Annual Research day at prestigious National Institute, JIPMER (Jawaharlal institute of Medical Education and Research) (JIPMER Newsletter Sep-Oct 2017).
- Vaswik National award for 2020 Vivdhalxi Audyogik Samshodhan Vikas Kendra Industrial research award: Conferred the award for biological sciences for the year 2020
PATENTS
Summary of Patents
| A compact-portable ambulatory video electroencephalography (VEEG) unit for seizure monitoring and comprehensive care for epilepsy patients (In Process)- Figure 6 | Dr P Sarat Chandra Dr Manjari Tripathi Kirandeep Kaur Amol Bhardwaj Anmol Gupta Dhananjay Goel | Indian Paten 201811033960 | 10.09.2018 |
| Implant system to enhance the cervico-occitial (cranio-vertebral junction) stabilization- commercialized with Medsolutions via FITT, IIT, Delhi- Figure 7- lower part | Dr P Sarat Chandra P Prarthana Chandra | Indian Patent 201911002700 | 22.01.19 |
| A disposable nasal retractor for endoscopic trans-sphenoidal pituitary gland surgery- commercialized with Walnut Medicals- Figure 9 | Dr P Sarat Chandra Kirandeep Kaur | Indian Patent 201911005181 | 09.02.19 |
| Disposable multi-port system for cranial endoscopic surgeries- In process for commercialization with Walnut Medicals | Dr P Sarat Chandra P Prarthana Chandra | 201911012505 | 23.03.19 |
| Novel techniques for reduction of basilar invagination and atlanto axial dislocation and surgical instruments thereof. The technique is in process with Medtronic (Mempis) for Commercialization of a universal spine reducer using this his, USA) as a industry-institute collaborative project- | Dr P Sarat Chandra AIIMS, Delhi | S20160128736A1 United States/ PCT patent US14/897,156 https://patents.google.com/patent/US20160128736 | 2014 |
Occipto-C1 and C2 spacer (Indian Patent Application No. 201611023116 dated July 5, 2016)
commercialized with Medtronics via AIIMS, Delhi- Figure 7- upper part | Dr P Sarat Chandra AIIMS, Delhi | Patent 201611023116 | July 5, 2016) |
| Designed a “disposable endoscopic carpal tunnel release set”- commercialized with AVM surgical via NRDC, Delhi | Dr P Sarat Chandra Dr Manjari Tripathi AIIMS, Delhi | Patent application no. 306/Del/ 2009 | 17.02.2009 |
| Designed a “special monopolar cautery”- Commercialized- AVM Surgicals | Dr P Sarat Chandra Nirmal Thakur AIIMS, Delhi | ||
| Multielectrode point radio frequency ablation device for performing bloodless epilepsy surgery | Dr P Sarat Chandra |
PUBLICATIONS RELATED TO NEW SURGICAL TECHNIQUES, INNOVATIONS AND PATENTS
Endoscopic Carpal Tunnel Surgery (Patented And Published)
- Patented this instrument for performing minimally invasive surgery for carpal tunnel syndrome, validate in over 200 patients
- Publication: Chandra PS, Singh PK, Goyal V, Chauhan AK, Thakkur N, Tripathi M. Early versus delayed endoscopic surgery for carpal tunnel syndrome: prospective randomized study. World Neurosurg. 2013, May-Jun;79(5-6): 767-72
Absolute Alcohol Injection With Short Segment Stabilization For Vertebral Body Hemangiomas:
- This is a unique technique of performing single stage absolute alcohol embolization of vertebral body haemangiomas along with single stage fixation.
- This technique showed excellent results on long term follow up for this otherwise very difficult to treat pathology. The cost of embolization is negligible (<1 USD!!) as compared to several lakh Rs. Required for traditional embolization.
- Papers on this material
- Chandra SP, Singh P, Kumar R, Agarwal D, Tandon V, Kale SS, Sarkar C. Long-term outcome of treatment of vertebral body hemangiomas with direct ethanol injection and short-segment stabilization. Spine J. 2019 Jan;19(1):131-143.
- Singh PK, Chandra PS (corresponding author), Vaghani G, Savarkar DP, Garg K, Kumar R, Kale SS, Sharma BS. Management of pediatric single-level vertebral hemangiomas presenting with myelopathy by three-pronged approach (ethanol embolization, laminectomy, and instrumentation): a single-institute experience. Childs Nerv Syst. 2016 Feb;32(2):307-14.
- Singh P, Mishra NK, Dash HH, Thyalling RK, Sharma BS, Sarkar C, Chandra PS (corresponding author). Treatment of vertebral hemangiomas with absolute alcohol (ethanol) embolization, cord decompression, and single level instrumentation: a pilot study. Neurosurgery. 2011 Jan;68(1):78-84; discussion 84.
Technique Of DCER For Craniovertebral Junction Surgery (Atlanto Axial Dislocation And Basilar Invagination)[60-65]
- The author developed this unique technique along with instrumentation for treating severe AAD and Basilar invagination. The technique allows surgeon to perform surgery using a single posterior approach and reduces morbidity and duration of surgery by > 50%.
- Patented for Developing a Universal CVJ reducer in collaboration with Medtronics (USA)
- Also developed a set of new instrumentation with a grant from Dept of Biotechnology, Ministry of Science & Technology, India.
- The surgical technique has been published widely and reduces complications, blood loss and hospital stay by over 50%
- The technique has been used in over 200 patients successfully and is now followed by surgeons all over the country
- Papers
- Joaquim AF, Tedeschi H, Chandra PS (corres author). Controversies in the surgical management of congenital craniocervical junction disorders - A critical review. Neurol India. 2018 Jul-Aug;66(4):1003-1015. doi: 10.4103/0028-3886.237025.
- Chandra PS, Prabhu M, Goyal N, Garg A, Chauhan A, Sharma BS. Distraction, Compression, Extension, and Reduction Combined With Joint Remodeling and Extra-articular Distraction: Description of 2 New Modifications for Its Application in Basilar Invagination and Atlantoaxial Dislocation: Prospective Study in 79 Cases. Neurosurgery. 2015 Jul;77(1):67-80; discussion 80.
- Chandra PS, Goyal N, Chauhan A, Ansari A, Sharma BS, Garg A. The severity of basilar invagination and atlantoaxial dislocation correlates with sagittal joint inclination, coronal joint inclination, and craniocervical tilt: a description of new indexes for the craniovertebral junction. Neurosurgery. 2014 Dec;10
- Chandra PS, Kumar A, Chauhan A, Ansari A, Mishra NK, Sharma BS. Distraction, compression, and extension reduction of basilar invagination and atlantoaxial dislocation: a novel pilot technique. Neurosurgery. 2013 Jun;72(6):1040-53; discussion 1053.
Endoscopic Hemispherotomy for drug resistant hemispheric epilepsy
- Developed a minimally invasive procedure for patients suffering from hemispheric drug resistant epilepsy- published in Epilepsia, Neurosurgery and Journal of Neurosurgery
- The surgery uses Robotic and endoscopic guidance and uses small incision (3 X 4 cm) as opposed to large craniotomy which was required prior to developing this technique. Reduces blood loss and morbidity as these surgeries are mostly performed in children (<9 years)
- This technique was demonstrated in patients by the author world over (various places in India as part of live surgical workshops, Malaysia, Morocco and Indonesia) and is now followed in several centers.
- Papers published
- Chandra PS, Subianto H, Bajaj J, Girishan S, Doddamani R, Ramanujam B, Chouhan MS, Garg A, Tripathi M, Bal CS, Sarkar C, Dwivedi R, Sapra S, Tripathi M. Endoscope-assisted (with robotic guidance and using a hybrid technique) interhemispheric transcallosal hemispherotomy: a comparative study with open hemispherotomy to evaluate efficacy, complications, and outcome. J Neurosurg Pediatr. 2018 Nov 9;23(2):187-197.
- Baumgartner JE, Blount JP, Blauwblomme T, Chandra PS. Technical descriptions of four hemispherectomy approaches: From the Pediatric Epilepsy Surgery Meeting at Gothenburg 2014. Epilepsia. 2017 Apr;58 Suppl 1:46-55. doi: 10.1111/epi.13679.
- Chandra SP, Tripathi M. Endoscopic epilepsy surgery: Emergence of a new procedure. Neurol India. 2015 Jul-Aug;63(4):571-82.
- Chandra PS, Kurwale N, Garg A, Dwivedi R, Malviya SV, Tripathi M. Endoscopy-assisted interhemispheric transcallosal hemispherotomy: preliminary description of a novel technique. Neurosurgery. 2015 Apr;76(4):485-94; discussion 494-5.
Endoscopic Corpus Callosotomy and Commisurotomy For Drug Resistant Epilepsy (Published In Neurosurgery):
- A minimally invasive technique developed by the author for the first time. The technique eliminated the need to do this surgery through a large craniotomy. In addition, the author for the first time demonstrated the role of commissures in Epilepsy and the value of cutting all the commissures in severe bi hemispheric epilepsy along with callosotomy
- Papers:
- Chandra SP, Kurwale NS, Chibber SS, Banerji J, Dwivedi R, Garg A, Bal C, Tripathi M, Sarkar C, Tripathi M. Endoscopic-Assisted (Through a Mini Craniotomy) Corpus Callosotomy Combined With Anterior, Hippocampal, and Posterior Commissurotomy in Lennox-Gastaut Syndrome: A Pilot Study to Establish Its Safety and Efficacy. Neurosurgery. 2016 May;78(5):743-51.
Robotic Guided Radio Frequency Ablative Disconnection Of Hyptothalmic Hamartomas Along With O-Arm Guidance
- The author developed this minimally invasive technique to treat hypothamic hamartomas presenting with gelastic epilepsy (laughing). These lesions are challenging to treat with open surgery
- The surgery can be performed using Robotic guidance along with O-arm registration
- Paper: Tandon V, Chandra PS (corresponding author), Doddamani RS, Subianto H, Bajaj J, Garg A, Tripathi M. Stereotactic Radiofrequency Thermocoagulation of Hypothalamic Hamartoma Using Robotic Guidance (ROSA) Coregistered with O-arm Guidance-Preliminary Technical Note. World Neurosurg. 2018 Apr;112:267-274. doi: 10.1016/j.wneu.2018.01.193. Epub 2018 Feb 3. PubMed PMID: 29408592.
A disposable nasal retractor for endoscopic trans-sphenoidal pituitary gland surgery- commercialized with Walnut Medicals- Figure 9
- Bajaj J, Chandra P S. Recent Developments in Endoscopic Endonasal Approach for Pituitary Adenomas. Neurol India 2020;68, Suppl S1:79-84
- Chandra P S, Kaur KD. Development of a Unique Retractor for Performing Endoscopic Pituitary Surgery-EASYTRAC. Neurol India 2019;67:1509-12
RELEVANT FIGURES

Figure 1: Shows various photographs in their respective timelines showing the establishment of MEG centre at National Brain Research Centre (NBRC). This centre has been established as a part of Centre of Excellence for Epilepsy as a collaborative project between AIIMS (New Delhi) and NBRC. Till date, more than 1700 MEG’s have been performed from all over the country and also from neighbouring countries like Bangladesh, UAE, and Nepal. All MEG’s are done completely free of cost.
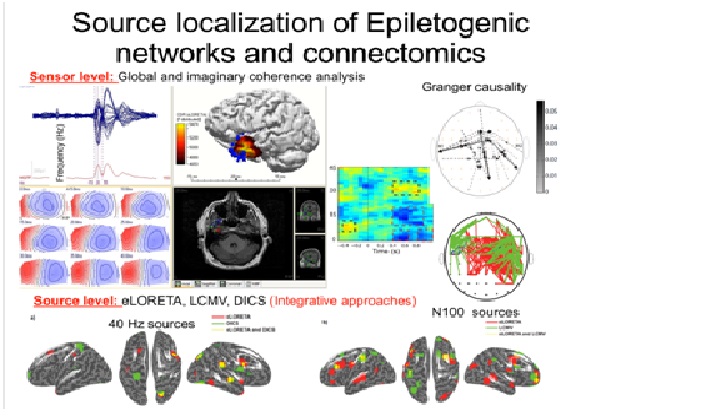
Figure 3: The following figure given below shows the capability of COE in creating advanced algorithms to localize epileptogenic networks. The networks are localized first by using MEG (using CURRY and S-Loretta software), followed by coherence studies which provides connectivity patterns in the brain. Coherence basically indicates identifying networks of neurons in the brain which fire at same frequency. There are reasons to believes based on Nominee’s studies that coherent neurons are connected with each other in patients with epilepsy. Such findings provide valuable insights to identify networks in persons with drug resistant epilepsy.
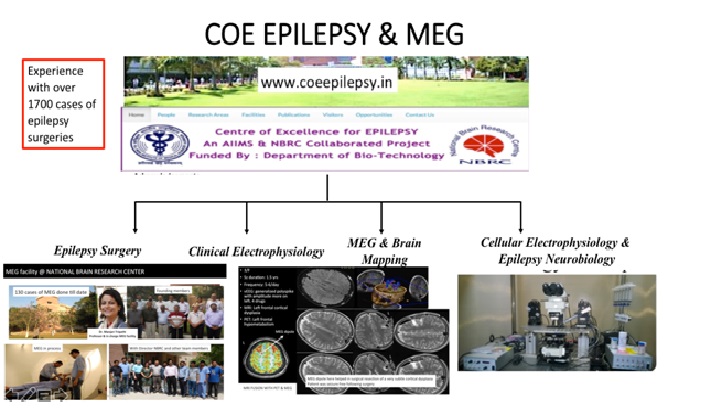
Figure 4: : The following figure shows the main components of the COE for which the Nominee is the PI and Team Leader. These include [1.] The Epilepsy surgery division [2.] Clinical Electrophysiology [3.] The MEG and Brain mapping centre located in the National Brain Research Centre [4.] Intra-cellular electrophysiology and molecular division. Such a multi-team and multi-speciality centre is the first of its kind for the country, and even for the whole South East Asia.
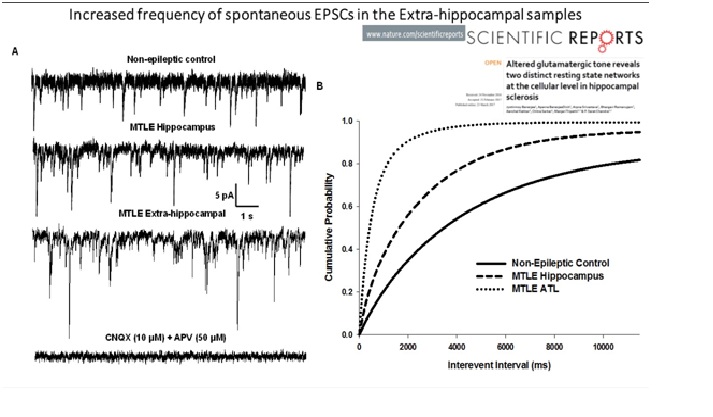
Figure 5: The following figure collage given below shows the capability of Cellular electrophysiology and Epilepsy Neurobiology lab (located in the convergence centre, AIIMS, named after Prof PN Tandon). This division has the capability of recording EPSC’s from live neurons provided from surgically resected brain samples which are carried to this lab within 10 minutes of surgical resection. This provides again valuable insights into connectivity patterns at the cellular and molecular level. The following figure collage given below is an excerpt from the publication in Scientific reports (Nature) which demonstrated for the first time, 2 separate networks, one from hippocampus and the other from the anterior temporal lobe. Such a finding provided immense translational value providing evidence at cellular level to perform an anterior temporal lobectomy + amygdalo-hippocampectomy as opposed to performing selective amygdalo-hippocampectomy. Such an evidence was earlier favoured by well known the meta-analysis performed by Josephson (Neurology, Impact factor 8.03). However, our study was the first of its kind to demonstrate this at the cellular level.
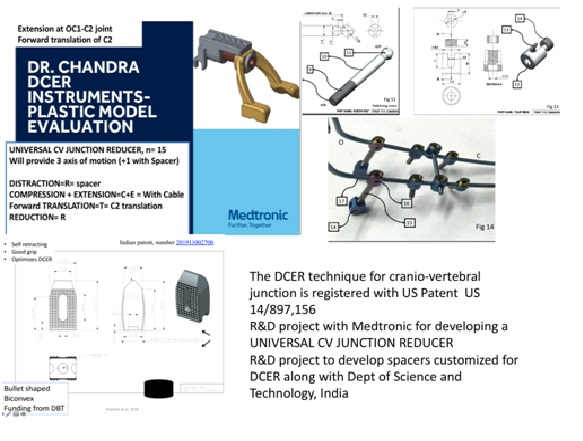
Figure 8: The technique of DCER for severe AAD and basilar invagination is patented, validated (>200 papers) and published. It is an established procedure which reduces operative time, morbidity, and hospital stay by> 50%. The nominee is also developing new implants and instrument in collaboration with DBT and Medtronics.
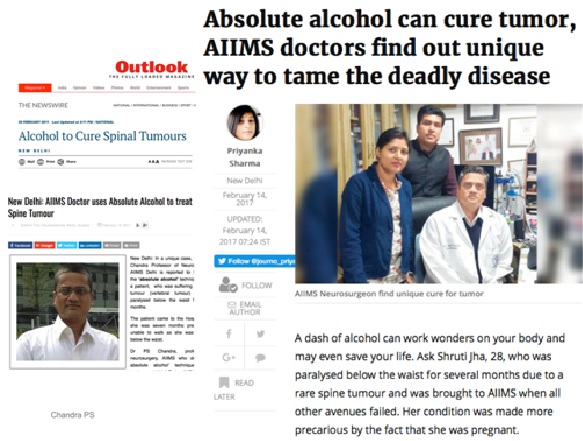
Figure 9: The technique of absolute alcohol embolization for vertebral hemangioma was published in several newspapers after it cured a young pregnant lady, wife of a reporter who came completely paraplegic during pregnancy. Following treatment, she became completely normal and delivered a normal healthy boy.
REFERENCES
Please SEE complete references (Total 392) at the end1-173174-392
Relevant papers mentioned here
- Dwivedi R, Ramanujam B, Chandra PS, Sapra S, Gulati S, Kalaivani M, Garg A, Chandra SB, Tripathi M, Dwivedi SN, Sagar R, Sarkar S, Tripathi M. Surgery for drug resistant epilepsy in children. New Engl J Med. 2017 377:1639-1647 Impact factor: 72.406 First RCT in Pediatric Epilepsy surgery in the world literature and first paper from India to be published in NEJM with all Indian authors with the study fully conceived and designed in India. I was the main and only surgeon to conduct the surgical cases.
- Banerjee J, Banerjee Dixit A, Srivastava A, Ramanujam B, Kakkar A, Sarkar C, Tripathi M, Chandra PS (corresponding author). Altered glutamatergic tone reveals two distinct resting state networks at the cellular level in hippocampal sclerosis. Sci Rep (Nature). (2017) 7(1):319. Impact factor: 4.259. This is seminal paper published in Nature (Sc reports) which for the first time in literature has demonstrated dual networks at a cellular level for generating epileptogenesis both from hippocampus and anterior temporal lobe. This is unlike the previous known literature where it was thought the epileptogenesis in hippocampal sclerosis originated only from the hippocampus. This paper throws light for the first time that an anterior temporal lobectomy with amygdalo hippocampectormy may have a better outcome than selective amygdalo-hippocampectomy.
- Baumgartner JE, Blount JP, Blauwblomme T, Chandra PS. Technical descriptions of four hemispherectomy approaches: From the Pediatric Epilepsy Surgery Meeting at Gothenburg 2014. Epilepsia. (2017), 1:46-55. Impact factor: 5.295.This paper provides technical description of the surgical technique “endoscopic hemispherotomy” developed by the author.
- Dixit AB, Banerjee J, Srivastava A, Tripathi M, Sarkar C, Kakkar A, Jain M, Chandra PS (corresponding author). RNA-Seq analysis of hippocampal tissues reveals novel candidate genes for drug refractory epilepsy in patients with MTLE-HS. Genomics. (2016) 107(5):178-88. Impact factor: 3.2. This paper explores new genetic marker as biomarkers to cause epilepsy.
- Chandra PS, Kurwale NS, Chibber SS, Banerjee J, Dwivedi R, Garg A, Bal C, Tripathi M, Sarkar C, Tripathi M. Endoscopic-Assisted (Through a Mini Craniotomy) Corpus Callosotomy Combined With Anterior, Hippocampal, and Posterior Commissurotomy in Lennox-Gastaut Syndrome: A Pilot Study to Establish Its Safety and Efficacy. Neurosurgery (Official journal of Congress of Neurological Surgeons, USA) (2016) 78(5):743-51. Impact factor: 3.6. The author has described this surgical technique for the first time in literature where a complete corpus callosotomy along with anterior, hippocampal and posterior commissurotomy has been described through a small incision of 3 cm size in patients who suffer from severe epilepsy with Lenox-Gestaut syndrome. Such a technique along with the combimation of corpus callostomy with commisurotomy has been described for the first time literature and has been shown to be significantly more efficacious than corpus callosotomy alone. In addition, the use of endoscopic technique has reduced the size of incision on cranium to just 3 cm size.
- Banerjee J, Banerjee Dixit A, Tripathi M, Sarkar C, Gupta YK, Chandra PS [corresponding author].Enhanced endogenous activation of NMDA receptors in pyramidal neurons of hippocampal tissues from patients with mesial temporal lobe epilepsy: A mechanism of hyper excitation. Epilepsy Res (2015); 117:11-6. Impact factor: 3.6. This paper correlated the hyperactivation of NMDA receptor to the excitability in pyramidal neurons in hippocampus of HS patients pointing to glutamatergic tone under resting conditions as a contributing factor in seizure generation
- Chandra PS, Prabhu M, Goyal N, Garg A, Chauhan A, Sharma BS. Distraction, Compression, Extension, and Reduction Combined With Joint Remodeling and Extra-articular Distraction: Description of 2 New Modifications for Its Application in Basilar Invagination and Atlantoaxial Dislocation: Prospective Study in 79 Cases. Neurosurgery (Official journal of Congress of Neurological Surgeons, USA). (2015) 77(1):67-80 Impact factor: 3.6.
- Chandra PS, Kurwale N, Garg A, Dwivedi R, Malviya SV, Tripathi M. Endoscopy-assisted interhemispheric transcallosal hemispherotomy: preliminary description of a novel technique. Neurosurgery (Official journal of Congress of Neurological Surgeons, USA). (2015) 76(4):485-94 Impact factor: 3.6. The paper for the first time in literatiure describes a new surgical technique of performing hemispheric disconnection using an endoscope. This technique was developed by the author at AIIMS and was performed as live surgery in many places in India and abroad (Malaysia, Morocco). The author also spoke about this technique in several lectures both in India and abroad. The technique provides a minimally invasive approach for a highly major surgical procedure usually performed in children, and thus reducing blood loss, hospital stay, morbidity and mortality significantly by more than 50%. The whole surgery is performed through a small incision of 4 cm size.
- Chandra PS, Vaghania G, Bal CS, Tripathi M, Kuruwale N, Arora A, Garg A, Sarkar C, Diwedi R, Malviya S, Padma V, Tripathi M. Role of concordance between ictal-subtracted SPECT and PET in predicting long-term outcomes after epilepsy surgery. Epilepsy Res. (2014) 0920-1211(14)00257-5. Impact factor: 3.6. This is the first paper in literature to demonstrate the use of concordance between SPECT and PET to predict long term outcomes of epilepsy surgery.
- Chandra PS, Ramdurg SR, Kurwale N, Chauhan A, Ansari A, Garg A, Sarkar C, Sharma BS. Extended costotransversectomy to achieve circumferential fusion for pathologies causing thoracic instability. Spine J. (2014) 14(9):2094-101.Impact factor: 2.8. This is one of the first study to demonstrate circumferential spinal fusion for 3 column instability
- Chandra PS, Goyal N, Chauhan A, Ansari A, Sharma BS, Garg A. The severity of basilar invagination and atlantoaxial dislocation correlates with sagittal joint inclination, coronal joint inclination, and craniocervical tilt: a description of new indexes for the craniovertebral junction. Neurosurgery (Official journal of Congress of Neurological Surgeons, USA). (2014) Suppl 4:621-9. Impact factor: 3.6 Papers 6.5 & 6.6 describe for the first time a new surgical technique for basilar invagination and atlanto-axial dislocation through a posterior only approach. The technique now performed in over 200 cases, may be used even in very severe cases of cranio-vertebral junction anomalies. This technique was demonstrated by the author is several live workshops both in India and abroad and the author also gave several lectures both in India and abroad. This technique has lead to 2 International patents and in terms of patient benefit has demonstrated 50% less morbidity and has cut down the hospital stay by more than half as compared to the traditional trans-oral excision of odontoid and posterior fixation. Paper 6.6 was the first paper from India to be ever published in Neurosurgery as editor’s choice.
- Chandra PS, Singh A, Goyal N, Laythalling RK, Singh M, Kale SS, Sharma MS, Suri A, Singh P, Garg A, Sarkar C, Sharma BS, Mahapatra AK. Analysis of Changing Paradigms of Management in 179 Patients with Spinal Tuberculosis Over a 12-Year Period and Proposal of a New Management Algorithm. World Neurosurg. (2013) Impact factor: 2.8.
- Chandra PS, Kumar A, Chauhan A, Ansari A, Mishra NK, Sharma BS. Distraction, compression, and extension reduction of basilar invagination and atlantoaxial dislocation: a novel pilot technique. Neurosurgery (Official journal of Congress of Neurological Surgeons, USA). (2013) 72(6):1040-53. Impact factor: 3.6. This paper describe for the first time in literature new indices for the C1/C2 joint which describe a new measure of severity of basilar invagination and atlanto-axial dislocation to plan surgical strategy
- Chandra PS, Bal CS, Jain S, Joshua SP, Gaikwad S, Garg A, Ansari A, Nehra A, Sarkar C, Tripathi M. Intra-Operative Co-Registration of MRI, PET and Electrocorticographic Data for Neocortical Lesional Epilepsies May Improve the Localization of the Epileptogenic Focus: A Pilot Study. World Neurosurg (official journal of World Federation of Neurosurgery). (2013) Impact factor: 2.8 This is the first ever paper to describe the concept of multi-modal imaging to localize the epileptogenic networks
- Chandra PS, Bal C, Garg A, Gaikwad S, Prasad K, Sharma BS, Sarkar C, Singh MB, Padma VM, Tripathi M. Surgery for medically intractable epilepsy due to postinfectious etiologies. Epilepsia. (2010). 51(6):1097-100 Impact factor: 5.295 This is the first ever study published in literature describing efficacy of epilepsy surgery for post infectious pathologies
- Chandra PS, Doddamani R, Girishan S, Samala R, Agrawal M, Garg A, Ramanujam B, Tripathi M, Bal C, Nehra A, Tripathi M. Robotic thermocoagulative hemispherotomy: concept, feasibility, outcomes, and safety of a new "bloodless" technique. J Neurosurg Pediatr. 2021 Apr 2:1-12. This is newly described technique of performing bloodless hemispheric disconnections using robotic guided multiple thermo-coagulations.
Technology Transferred/Patents, If any. (Stating whether patents were commercialized)
- The technique of Distraction, compression, extension and reduction (DCER) along with the relevant instrumentation to perform the technique. (Patent pending with US registered with number US patent 14/897,156)
- The technique describes a new technique of reducing and aligning severe irreducible basilar invagination and atlanto-axial dislocation through a posterior approach only
- Reduces the morbidity and operating time by 50%
- The patent describes the technique and also set of unique instrumentation to perform the procedure using the standard implants
- Following the patent, 3 papers published in NEUROSURGERY
- Commercialization of a universal spine reducer using this technique is in process with Medtronic (Memphis, USA) as a industry-institute collaborative project
- Commercialized- Medtronics
- Occipto-C1 and C2 spacer (Indian Patent Application No. 201611023116 dated July 5, 2016)
- Unique implant which allows placement between the O-C1 and C2 joints
- Customized to perform the DCER technique to reduce basilar invagination and atlanto-axial dislocation
- Unique design allows self retraction of the joint surfaces
- Currently being developed as under support from BIRAC (DBT, Ministry of Science and Technology, India)
- Commercialized- Medsolutions
- Designed a “disposable endoscopic carpal tunnel release set”(Patent application no. 306/Del/2009 dt. 17.02.2009
- Used it successfully in 200 patients [patent filed]. In commercial production
- Device is low cost, made of recycled hard plastic, “use and throw”, costs less than 10 USD for one device
- Paper published in world neurosurgery
- Commercialized- AVM Surgicals
- Designed a “special monopolar cautery”
- For use in trans-oral surgery for CV Junction anomalies. Used it successfully in more than 100 cases [patent accepted and filed].
- Published in Indian Journal of Neurosurgery
- Commercialized- AVM Surgicals
- EPISAVES: Epilepsy Patient Integrated Automated Video EEG System: A portable first of its kind of video EEG system being developed with AI integration being developed with a grant from PSA (Principle Scientific Advisor) office- patented Indian Paten 201811033960
- “Multielectrode point radio frequency ablation device for performing bloodless epilepsy surgery” patented
- “EASYTRAC” A unique retractor for performing endoscopic pituitary surgery Chandra PS, Kaur KD. Development of a Unique Retractor for Performing: Endoscopic Pituitary Surgery-EASYTRAC. Neurol India. 2019 Nov-Dec;67(6):1509-1512. doi: 10.4103/0028-3886.273609. PubMed PMID: 31857547.- patented
- A disposable nasal retractor for endoscopic trans-sphenoidal pituitary gland surgery- commercialized with Walnut Medicals- Figure 9-
Papers published:- Chandra P S, Kaur KD. Development of a Unique Retractor for Performing Endoscopic Pituitary Surgery-EASYTRAC. Neurol India [serial online] 2019 [cited 2020 Nov 22];67:1509-12. Available from: https://www.neurologyindia.com/text.asp?2019/67/6/1509/273609
- Bajaj J, Chandra P S. Recent Developments in Endoscopic Endonasal Approach for Pituitary Adenomas. Neurol India 2020;68, Suppl S1:79-84
- Disposable multi-port system for cranial endoscopic surgeries- In process for commercialization with Walnut Medicals. Patent: 201911012505
Contribution to National/International issues; If any.
- President Elect, Indian Epilepsy Society (IES)
- Treasurer, Neuro endoscopic Society of India
- President, Skull Base Surgery Society of India
- Past Secretary, Skull Base Society of India (www.sbssi.org)
- Past Hon’ble Treasurer of Neurological Society of India
- Past President of Asian Congress of Epilepsy Surgery (AESC)
- Member, Commission for Pediatric Epilepsy Surgery, International League against Epilepsy (ILAE)
- Faculty 1000, ILAE
- Founder member, Ekatwam (Standing up against epilepsy) (www.ekatwam.org)
- Principal investigator of Prof PN Tandon Neurobiology lab: housed in the convergence center at AIIMS has advanced facilties to perform molecular and cellular electrophysiological work. This has the only facilty in the entire South Asia to perform single cell intra cellular electrical recordings
- Editor, Neurology India, Impact factor 2.7 since 2019
- Have been assigned as the Nodal Person In Charge of Developing Countries for Epilepsy Surgery, from International League Against Epilepsy (https://www.ilae.org/p-sarat-chandra)
- Designated by ILAE to develop Epilepsy Surgery Data Base Pan Asia
- Designated as the key person in Charge to develop Epilepsy Surgery Sensitization and Education Programs for Bhutan and Nepal (by conducting workshops in the year March 2020)
Papers presented in conferences (online conferences to be updated):
| Conferances, Guest Lectures & Visiting Professor: | |||
|---|---|---|---|
| S. No. | Conference Title/Agenda | Year | Venue |
| 1 | Indian Epilepsy School 2019 – Faculty Presented 2 lectures of 1.] Disconnective Epilepsy Surgery 2.] Resective Epilepsy Surgery | 22nd to 25th Aug 2019 | Jodhpur |
| 2 | Korean Cervical Spine Research Society-13th Annual Meeting of the Korean Cervical Spine Research Society Presented Key note Oration Reducing severe AAD and BI using the DCER principle | 8th June 2019 | Korea |
| 3 | 3rd International Conference on Clinical Spine & Orthopedic BIOMECHANICS Presented on the biomechanics of Cranio vertebral junction | 26th to 28th April 2019 | New Delhi |
| 4 | American Association of Neurological Surgeons Presented Invited lecture symposium on “ Endoscopic Hemispherotomy: From Concepts to Practice” | 13th to 17th April 2019 | San Diego |
| 5 | 11th Annual Conference CME Credit Hours 2 – MPMC/CME-08/2019/505 | 4th April 2019 | Bhopal |
| 6 | NEURO ENDOCON 2019 Invited faculty: gave lecture on Endoscopic management of Large Intra ventricular tumors | 29th to 31st March 2019 | Madurai, Tamil Nadu |
| 7 | CAWNPORE NEUROLOGICAL SOCIETY 2019, Kanpur Guest Faculty in UP-UK-NEURON 2019 | 2nd & 3rd February 2019 | Kanpur |
| 8 | ASSICON 2019-32nd Annual Conference of Association of Spine Surgeons of India Invited Faculty | 24th to 27th January 2019 | Ahmedabad |
| 9 | 15th Instructional & 9th Foundation Course participated as Faculty organized by Neurological Society of India | 12th & 13th January 2019 | Cuttack, Orissa |
| 10/td> | 4th ASSICON, International Congress on Minimal Invasive Neurosurgery Faculty | Jan, 19-21, 2018 | Chennai, India |
| 11 | AIIMS Microneurosurgery Workshop Faculty, Gave live surgical demonstration | Feb 15-17, 2018 | AIIMS, New Delhi |
| 12 | NESON, Nepal Faculty and lecturer | Mar 5-7, 2018 | Nepal |
| 13 | NEUROCON, Nagpur Faculty, presented multiple lecutures | Apr, 1-5, 2018 | UP, India |
| 14 | Annual Congress on Skull Base Surgery(SBSSI) Faculty | Apr, 4-6, 2018 | Chennai, India |
| 15 | 2nd ASSI (Association of Spinal surgeons of India) Conference, Faculty | May, 8-9, 2018 | New Delhi, India |
| 16 | Indian Epilepsy Society Conference Faculty | May, 18-19, 2018 | New Delhi, India |
| 17 | ISC (Instructional Spine Course) Faculty | July, 9-10, 2018 | Amritsar, Punjab, India |
| 18 | Neurotrauma Conference Faculty | Aug, 16-19, 2018 | AIIMS, New Delhi, India |
| 19 | 13th European Congress on Epileptology Presented paper on “Endoscopic hemispherotomy” Faculty | Aug, 26-30, 2018 | Vienna, Austria |
| 20 | Neurovision Faculty | Oct, 9-10, 2018 | Bhubaneswar, Orissa |
| 21 | Congress of Neurological Surgeons, Annual Meeting Faculty | Oct, 5-9, 2018 | Houston, Texas |
| 22 | 52nd Congress of Japanese Epilepsy Society Faculty Invited Oration: Optimizing Surgical Strategies to make Epilepsy Surgery affordable in Developing Countries. | Oct, 23-24, 2018 | Yokohama, Japan |
| 23 | 12th Asian Epilepsy Surgery Conference Faculty | Oct, 26-27, 2018 | Bali, Indonesia |
| 24 | 15th EEG workshop and Masterclass in Epilepsy -Organiser, presented multiple lectures on Epilepsy Surgery and EEG | Nov, 22-24 | Varanasi, UP |
| 25 | 67th Annual Conference of the Neurologocal Society of India Faculty | Dec, 13-16, 2018 | Jaipur Rajasthan |
| 26 | Neurological Society of India annual congress -Chaired session on cranio-vertebral junction anomalies -Spoke on Endoscopic hemispherotomy | 30th Nov-2nd December, 2017 | Nagpur, India |
| 27 | Asian Epilepsy surgery congress - Participated as board member - Gave lecture on the following topics - Robotic radiofrquency ablation of hypothalamic hamartomas - Endoscopic hemispherotomy - First Radomized trail for Pediatric epilepsy surgery published in NEJM | 17-19th, November, 2017 | Shanghai, China |
| 28 | Annual Skull Base Surgery congress -Participated as secretary general -Lecture on Trans-septal endoscopic robotic approach to supra sellar lesions and tumors | 27-29th October, 2017 | Cochin, India |
| 29 | 76th Annual congress of neurological surgeons of Japan - Gave luncheon seminar on “Epilepsy surgery” - Spoke on “Endoscopic hemispherotomy” | 13th October, 2017 | Nagoya, Japan |
| 30 | CNS-Boston- Faculty, Participated in the following events - Moderated the symposium on minimally invasive epilepsy surgery and spoke on endoscopic hemispherotomy - Talk on Utilizing the DCER priniciple to reduce severe basilar invagination and atlanto axial dislocation | 8-11th October, 2017 | Boston, USA |
| 31 | NEUROVASCON: Faculty: Clipping techniques of complex posterior aneurysms | 15-17th Septermber, 2017 | Delhi, India |
| 32 | Epilepsy Surgery Update: Participated in this congress as the Chief faculty, provided several lectures and performed live surgery | 23rd July, 2017 | Surabaya, Indonesia |
| 33 | Asian Congress of Neuro Surgeon Congress (ACNS) Participated as faculty and presented paper on- Eyebrow keyhole mini-fronto orbital craniotomy approach to anterior circulation aneurysms | 19-22nd July, 2017 | Indonesia |
| 34 | INI International Neurosurgical Congress, Hannover. Participated as faculty and presented paper on “Endoscopic hemispherotomy and corpus callosotomy” | 16-19th June, 2017 | Hannover, Germany |
| 35 | SPINE Update: Participated as faculty and presented on the DCER principle for CV junction anomalies | 30th April, 2017 | Vadodara, Gujrat |
| 36 | Neurosurgery Update: Participated as faculty and presented on endoscopic hemispherotomy | 15-16th April, 2017 | Agra, India |
| 37 | Neuroendocon annual congress, Participated as faculty and presented on -Endoscopic hemispherotomy -Robotic guided trans-septal approach to pituitary tumors | 7-8TH April, 2017 | Jaipur, India |
| 38 | Ginde oration: Mumbai Delivered guest lecture and operated a live surgery on endoscopic hemispherotomy as part of the CME operative workshop | 22n-23rd March, 2017 | Mumbai, India |
| 39 | CTRF: AIIMS, Delhi, Participated as faculty and gave hands on demonstration on DCER technique for CV Junction | 19th March, 2017 | AIIMS, New Delhi |
| 40 | NESON: Nepalese neurosurgical society annual meeting; Participated as faculty and presented a paper on “Strategies to localize epileptogenic networks” | 10th March, 2017 | Kathmandu, Nepal |
| 41 | Clinical Spine Biomechanics: Participated as faculty and presented “Biomechanics of CV Junction | 4th March, 2017 | ISIC, Delhi |
| 42 | Faculty and gave a lecture at the Epilepsy Congress on : Epilepsy networks for planning surgical strategies | 17-19th February, 2017 | Patna, India |
| 43 | Visiting Professor, Univerisity hospital, Kuala Lumpur, Malaysia. Performed a live operative case of endoscopic hemispherotomy | 1st-3rd, December, 2016 | Kula Lumpur, Malaysia |
| 44 | Indian Epilepsy School. Participated as faculty and presented the following topic: Advances in surgical strategies to localize epileptogenic networks | 25-27th, November, 2016 | Ludhiana, India |
| 45 | 24th Annual congress of Indian Academy of Neurology. Participated as faculty and presented the following lecture 1.) Neuromodulation techniques to manage drug refractory epilepsy | 11th November, 2016 | Kolkotta, India |
| 46 | Neurovision, a CME on neurosciences. Participated as guest faculty and spoke on following topics 1.) Strategies to localize epileptogenic networks 2.) Management of low grade gliomas in eloquent cortical regions | 10th, November, 2016 | Bhubanesar, Odisha |
| 47 | Epilepsy Surgery Symposium, participated as faculty and presented the following topics 1.) The utility of MEG for localization of epileptogenic networks 2.) Use of robotic SEEG to localize epileptogenic networks following a robust hypothesis following video EEG, SPECT, PET, and MEG 3.) Endoscopic hemispherotomy | 7-8th November, 2016 | Bangalore, India |
| 48 | Asian Epilepsy Surgery Congress, participated as President and presented the following lectures 1.) Endoscopic disconnection techniques 2.) Development of Epilepsy surgery in India | 4-5th, November, 2016 | Incheon, Korea |
| 49 | Visiting Professor, University hospital Rabat, Morocco: Operated 2 cases of hemispherotomies and presented several papers on epilepsy surgery and pre-surgical localization techniques. This was the first time that hemispherotomy was performed in Morocco | 23rd-28th, October, 2016 | Rabat, Morocco |
| 50 | International Spine and spinal injuries congress, participated as faculty and presented the following paper “Reduction of old C2 fractures using DCER principle” | 6-8th October, 2016 | Kathmandu, Nepal |
| 51 | 27th Annual INDSPN conference & ISPN CME, participated as faculty and presented “Newer strategies for pediatric epilepsy surgery” | 1-4th October, 2016 | AIIMS, New Delhi |
| 52 | Asia Spine Congress, Participated ad faculty, presented the following paper “Reducing severe cranio-vertebral junction deformity using DCER principle” | 22-24th September, 2016 | Seoul, Korea |
| 53 | Epilepsy Surgery Techniques, conducted by International League against epilepsy Presented the following paper as faculty “Endoscopic hemispherotomy” | 17th September, 2016 | Prague, Czeh Republic |
| 54 | SKULL BASE CON 2016, Participated as the general secretary of SBSSI and also presented the following lecture “Reduction of severe deformity, decompression of the spinal canal and stabilization of severe AAD and basilar invagination using the DCER principle” | 8-11th September, 2016 | Jaipur, India |
| 55 | CME on Endoscopic techniques for epilepsy surgery- Participated as the only Chief faculty and demonstrated a live operative case of endoscopic hemispherotomy | 23-28th August, 2016 | Kulala Lumpur, Malaysia |
| 56 | Advanced spine workshop- Participated as faculty, gave lecture on “Reduction of severe AAD and basilar invagination using the DCER principle”. Demonstrated live operative cases of severe basilar invagination | 13-14th August, 2016 | AIIMS, Delhi |
| 57 | CME on Epilepsy update- Participated as faculty presented lectures on epilepsy surgery and operated 2 cases of mesial temporal sclerosis as live surgical demonstration | 6-7th August, 2016 | Surat, India |
| 58 | ASRAM neurocon-2016- Participated as faculty, presented various surgeries and performed live operative cases of endoscopic CSF repair and acoustic schwanomma | 29-31st July, 2016 | Eluru,India |
| 59 | CME on craniovertebral junction anomalies. Faculty- presented various lectures and demonstrated a live operative case | 22-23rd July, 2016 | Jabalpur, India |
| 60 | 3rd Walter Dandy Educational course- Faculy, Presented the following lectures -Vascular bypass techniques - Micro surgical clipping of Acom aneurysms | 14-16th July, 2016 | Udaipur, India |
| 61 | 7th India-Japan Neurosurgical conference- Presented the following topic- Endoscopic disconnective techniques for epilepsy surgery | 18-20th June, 2016 | Osaka, Japan |
| 62 | 6th International Neurosurgery update and educational initiative of the Asian Australian Sociaty of Neurological Surgeons. Participated as faculty, gave the following lecture- Surgical strategies to manage gliomas located in eloquent regions | 4-5th June, 2016 | Mumbai, India |
| 63 | Participated as faculty and conducted the following activities -Chairperson for plenary session -Lecture given “Determinants for epilepsy surgery outcomes” | 28-29th May, 2016 | EPILEPSY CONCLAVES, Pune, India |
| 64 | Participated as faculty, gave the following plenary lecture - Endoscopic applications of Epilepsy surgery - Co-author for paper “The role of MEG propogation to localize the epileptogenic networks” | 15th, May, 2016 | Asiano-Oceanic Epilepsy Comission Congress, ILAE, Hong Kong AOEC is the largest congress of this region for Epilepsy. |
| 65 | Participated as faculty -Operated live surgery of a case with severe basilar invagination and atlanto axial dislocation -Gave a lecture on “The technique of DCER for correcting BI, AAD and deformity” | 6-8th, April, 2016 | AIIMS, New Delhi |
| 66 | Conducted a cadaveric workshop and delivered 2 guest lectures on a workshop for Cranio-vertebral junction anomalies -Trans laminar screw fixation and occipito-cervical fixation -The technique of DCER for cranio-vertebral junction anomalies surgery | 23-24th, April, 2016 | PGIMER, Chandigarh |
| 67 | Delivered the following plenary lectures -Endoscopic applications in Epilepsy Surgery -Localizing epileptogenic networks for planning surgical strategy | 17-19th April, 2016 | 5th Symposium of World Federation of Neurosurgical Societies (WFNS) and MASSIN interim meeting, Tehran, Iran |
| 68 | Participated as faculty, delivered the following lectures - Endoscopic applications for epilepsy surgery - Endoscopic excision of intraventricular tumors | 15-16th April, 2016 | 3rd Neuroendoscopic conference, AIIMS, New Delhi |
| 69 | Delivered the following guest lectures -Basilar invagination, incidence and management -Complication avoidance in cranio-vertebral junction surgery with case vignettes | March, 2016 | Spine Summit (Joint congress of CNS, NASA) Orlando, US |
| 70 | Delivered the following guest lectures -A new technique to reduce basilar invagination and atlanto axial dislocation -Plenary session: Overcoming barriers of epilepsy surgery in resource poor countries | March, 2016 | 11th Asian Congress of Neurosurgeons Society (ACNS), Surabaya, Indonesia |
| 71 | Demonstrated Live Surgery of DCER in congenital basilar invagination and atlanto axial dislocation | March, 2016 | Live Annual Microneurosurgery workshop, AIIMS, New Delhi |
| 72 | Dr AD Sehgal Oration; Annual Epilepsy Congress (Indian Epilepsy Society): Creating Cost effective and efficacious strategies for Epilepsy Surgery for Inida | February, 2016 | Annual Epilepsy Congress (Indian Epilepsy Society): Vishakapatnam |
| 73 | Guest Lecture: Endoscopic Epilepsy Surgery | December 2015 | Annual Congress of Neurological Society of India, Hyderabad |
| 74 | Guest lecture: Complication avoidance in craniovertebral junction surgery | December, 2015 | Annual Congress of Spinal Surgeons of India, Goa |
| 75 | Guest lecture: The technique of DCER to reduce basilar invagination and atlanto axial dislocation through a posterior only approach | 16-18th November, 2015 | Annual Skull Base Congress, Bangalore |
| 76 | Guest lecture: Applying the law of levers to reduce basilar invagination and atlanto axial dislocation. | 05/2015 | ANEICON, ORISSA; |
| 77 | Guest lectureApplying the law of levers to reduce basilar invagination and atlanto-axial dislocation: Description of a new technique. | 04/2015 | Asian Australasian Congress of Neurological Surgeons, Juju Island, Korea; |
| 78 | Organized the "Advanced Epilepsy Surgery, Epilepsy Neurobiology and functional workshop". Advanced Epilepsy Surgery, Epilepsy Neurobiology and functional workshop, | 04/2015 | AIIMS, New Delhi, |
| 79 | Organised the advanced Epilepsy Surgery, functional and pain workshop-9-11th April, 2015. Organised the advanced Epilepsy Surgery, functional and pain workshop- | 9-11th April, 2015; 04/2015 | AIIMS, New Delhi, |
| 80 | Disconnective epilepsy surgery: paper presented as invited faculty at the EPILEPSY CONCLAVE. | 04/2015 | Hyderabad; |
| 81 | Pondicherry neurosciences club, presented an oration on “Creating a successful epilepsy surgery program | 4th January, 2015 | Pondicherry |
| 82 | Chief faculty at the JIPMER cranio vertebral junction anomalies cadaveric workshop, presented 2 lectures as a faculty | 2-4th January, 2015 | Pondicherry |
| 83 | Giant MCA aneurysm-How I do it?, Applying the law of levers for reduction of basilar invagitation and AAD, Faculty and EC member of NSI CON 2014 | 10-14TH December, 2014 | Coimbatore |
| 84 | Posterior cervical spine solutions: Partcipated as faculty in this hands on spine workshop | 28-29th, September, 2014 | Bangalore |
| 85 | Indo-American Spinal Alliance (IASA) hands on spine workshop for cervical spine: Partcipated as a faculty presented the lecture: Surgical concepts of C1-C2 fixation | 26-27th September, 2014 | Bangalore |
| 86 | Annual congress of neurospinal surgeons society congress. Ahmedabad, presented the papers - Management of intra medullary spinal tumors in AO spine symposium - Evolving paradigms in management of basilar invagination and atlanto-axial dislocation | 21st September, 2014 | Ahmedabad |
| 87 | VHS annual microneurosurgery workshop. Participated as a Chief faculty in this live operative workshop. Received felicitation from His Excellency, Abdul Kalam, former President of India for the same | 18-20th, September, 2014 | Chennei |
| 88 | 9th Asian Epilepsy Surgery Congress. Presented the following paper “Endoscopic hemispherotomy: From concepts to practice”. Participated as faculty | 3rd-7th October, 2014 | Tokyo, Japan |
| 89 | Annual congress for Instructional course in spine. Presented the paper “Osteoarthritis of CV Junction” | August, 2014 | Udaipur |
| 90 | 10th AOEC, Singapore: Presented the following paper in ASEPA teaching course “Multimodal imaging and epileptogenic networks” and participated as a faculty | 7-9th August, 2014 | Singapore |
| 91 | Epilepsy Conclave 2014 | 12-13th Jul, 2014 | Goa, India |
| 92 | Post Pediatric Epilepsy Meeting | 4-5th Jul, 2014 | Gothenburg, Sweden |
| 93 | European Congress on Epileplogy (ECE) | 29th Jun to 3rd Jul, 2014 | Stockholm, Europe |
| 94 | Complex Spine Trauma, JPNA Trauma Centre. Faculty, gave didactic lectures and demonstrated live surgeries | 11th & 12th May 2014 | AIIMS, New Delhi |
| 95 | NSI Conference Curriculum Course: Conducted this course with senior members of NSI at AIIMS and created an uniform guidelines for neurosurgical curriculum | 15th March 2014 | AIIMS, New Delhi |
| 96 | NSI Teaching Program | Feb, 2014 | Kolkatta |
| 97 | AIIMS Microneurosurgery Workshop | 21st to 23rd Feb 2014 | JPNA Trauma Centre, New Delhi. |
| 98 | Rammiah, Banglore: Faculty for cervical spine hands on cadaveric course at MSR advanced facility for cadaveric training | Feb 2014 | Banglore |
| 99 | -Invited faculty: Presented the following talk: “Epileptogenic networks and the Epilepsy Surgeon” | 24-27th October | 7th Asian Epilepsy Surgery Congress, Beijing |
| 100 | Techniques of Epilepsy surgery- Invited lecture Chief faculty for 3D cadaveric workshop for epilepsy Invited faculty for “1st National Functional congress and cadaveric workshop” | September, 2013 | 1st National Stereotactic and Functional cadaveric workshop, Surabaya, Indonesia |
| 101 | “Distraction, compression extension and reduction” Deription of a new novel technique for reduction of BI and AAD “Developing customized treatment paradigms for pharmacoresistant epilepsy in developing countries” Presented the above papers as a invited faculty at WFNS, Seoul, Kore | September, 2013 | WFNS, Seoul, Korea, |
| 102 | “Long term outcome in persons with drug refractory epilepsy after resection in unilateral mesial temporal sclerosis” Poster presented. | June 23-27th, 2013 | Montreal International Epilepsy Congress, Canada |
| 103 | Presidential Symposium “Epilepsy Focus: Is It a Zone or a Network? | June 13-15th, 2013 | Korean Epilespy Congress, Korea |
| 104 | Presented Paper “Distraction, compression, extension and reduction for basilar invagination and atlanto-axial dislocation- a new novel technique” | April 4-6th, 2013 | Global Spine Congress, Hong Kong |
| 105 | Chairman of the operative workshop conducted at the Calicut govt college on cranio-vertebral junctions-“The juncture” delivered a lecture on newer techniques on management of craniovertebral junction anomalies. | Feb 28th, 2013 | Calicut govt medical college |
| 106 | Recent advances in molecular mechanisms of neurological disorders, Faculty and invited speaker: “Epileptogenic networks and epileptogenic focus: Role of multimodal imaging”. | Feb 22nd, 2013 | AIIMS, New Delhi |
| 107 | 1st Indo-German meeting for NEUROBIONICS: Faculty, presented guest lecture on “Role of electrical stimulation for bladder and bowel disorders”. Moderated the session on “Role of VNS and other electrical stimulation modalities for epilepsy” | Feb 16th, 2013 | JIPMER, Pondicherry |
| 108 | Joint Neurosurgical Convention, 6th International Mt Bandai symposium for Neurosciences, The 7th Pan Pacific Neurosurgery congress Was an invited guest faculty and presented at the main penary session “Distraction, Compression, Extension and reduction of Basilar invagination and atlanto axial dislocation: Description of a new nove technique“. | Jan 29th-Feb 4th, 2013 | Hawai, USA |
| 109 | Advanced workshop on epilepsy surgery Faculty, gave a lecture on “Pediatric Temporal Epilepsy surgery” and participated as a faculty | 5-6th, January, 2012 | Kochi, Kerela |
| 110 | 61st Annual National Congress of Neurological Society of India, Delhi NCR Organizing secretary Conducted the CV Junction symposium and gave a lecture on intra operative manupilations to reduce basilar invagination and AAD Gave a lecture on posterior circulation aneurysms Moderated the “meet the expert” symposium and presented a case on “Status epilepticus in a neonate” | 17th-22nd December, 2012 | Delhi, NCR |
| 111 | 6th Asian Epilepsy Surgery Congress, Busan Korea. Participated as a faculty, and Board member of AESC. Presented the paper “Pediatric epilepsy surgery from India- Investigations, Outcome and QOL” | 8-10th, November, 2012 | Busan, Korea |
| 112 | ISPN Annual congress: held at AIIMS; Vice Chairman for scientific committee; gave two lectures: 1) Role of spacers and jammers in CVJ anomalies 2)Hemispherotomy for epilepsy surgery | 31-2nd Nov, 2012 | AIIMS |
| 113 | First instructional course on CV Junctions anomalies: GB Pant Medical college, New Delhi, 12-13th, October, 2012. Participated as a faculty and spoke on “Spacer distraction and extension to reduce AAD and BI” | 12-13th October, 2012 | GB Pant Medical college, New Delhi |
| 114 | International Spine and Spinal injuries conferences (ISICON), 12-14TH October, 2012. Participated as faculty; Panelist on workshops on “Metastatic spinal tumors” and “Cervical myelopathy” | 12-14th October, 2012 | Indian Spinal injuries center, New Delhi |
| 115 | Fundamentals of spine surgery: Hands on spine workshop on basics of spine surgery. Conducted this workshop and gave lectures on management of CVjunction, spondylolisthesis, and anterior cervical approach. Also provided hands on workshop training for spine instrumentation. Course conducted by Academia for spine education, Medtronic. | 29-30th Sept, 2012 | New Delhi, Hotel Claridges |
| 116 | ICVS: Annual congress of cerebraovascular society Participated as faculty, Chaired and participated as a panelist in the CME on 21st and presented a paper on 23rd on “mini-orbito-fronatal craniotomy for anterior cirucaltion aneurysms” | September, 21-23rd, September, 2012 | Mumbai |
| 117 | Spine 2012, Annual congress of Neurospinal surgeons society of India (NSSA) Was faculty and National coordinator for this congress Chaired and participated as a panelist on the session for bio-informatics for spine surgery, spoke on the following topics (1) Distractive compressive extensive reduction for basilar invagination and atlanto axial dislocation- a new novel technique (2) Cervical vertebral tumors | September, 13-15th, 2012 | Chennei |
| 118 | ICS-2012, Official congress of the ASSICON Was National Faculty- presented 2 papers 1) Video on cervical spacer jamming 2) Panel discussion of a difficult case of cervical tumor | August 13-16th, 2012 | Srinagar |
| 119 | Total cervical spine solution: Conducted this workshop on cervical spine with hands on models and gave 3 lecture: cervical arthroplasty, cervical trauma, cervical spine stabilization | July, 14-15th, 2012 | New Delhi |
| 120 | Chief faculty, Video spine symposium, Ahmedabad orthopedic association, Ahemedabad Delivered 2 video lectures: Cervical arthroplasty, and TLIF for lumbar spine fusion | July, 9th, 2012 | Ahmedabad |
| 121 | Guest faculty: Cleveland Clinic Kokilaben Epilepsy symposium, | May 2012 | Mumbai. |
| 122 | Guest faculty: Presented a lecture on "Management of cervical spine tumors", | March 2012 | ASSICON, New Delhi. |
| 123 | Guest faculty:, presented a lecture "Epilepsy surgery" in the Epilepsy surgery symposium | March 2012 | NSSI conference, Pune. |
| 124 | Guest lecture: research paradigms for epilepsy surgery. | April; 2012 | Bombay Neurological Association |
| 125 | Presented the following papers in the NSI annual congress held in Bangalore: (1) Key hole approach to aneurysms (2) Basilar top aneurysms: how I do it video session (3)Best paper for CeibaGiegi Epilepsy award paper | 2011; December | NSI annual congress held in Bangalore |
| 126 | Pediatric epilepsy surgery with QOL: Experience with 130 cases; | 2011; October | ISPN, Goa |
| 127 | In hospital management of epilepsy: Lecture for nursing symposium | 2011; October | ISPN, Goa |
| 128 | Participated and presented cases as a faculty in the Epilepsy surgery symposium | 2011; October | ISPN, Gos |
| 129 | Challenges in pediatric epilepsy surgery | 2011 | ILAE |
| 130 | Faculty, Consensus for providing guidelines for pediatric epilepsy surgery | 2011 | ILAE, Rome 2011 |
| 131 | Challenges in pediatric epilepsy surgery, experience with 150 cases. | 2011 | ILAE congress, Rome, 2012 |
| 132 | Faculty and Secretary General, Asian Epilepsy Surgery Society. | 2010 September | Annual International congress, Taipei |
| 133 | Guest faculty, King Fahad Hospital, Saudi Arabia; International Medical Symposium sponsored by the Ministry of Health and His Royal Highness King Mohammad Bin Saud: Gave 2 lectures: “Keyhole Cranio orbital approach to aneurysms” & “Surgery for Intractable Epilepsy”. | 2010 | King Fahad Hospital, Saudi Arabia; International Medical Symposium |
| 134 | ISSICON; International Spine and Spine Injuries: Invited Faculty; delivered guest lecture; Management of Vertebral body haemangiomas. | 2009 | ISSICON |
| 135 | Presented paper on “Intraoperative absolute alcohol embolization for vertebral body haemangiomas. | 2009 September | WFNS, Boston |
| 136 | Faculty, National, AO Spine, AO Spine Principles Course. | Jul-09 | New Delhi |
| 137 | Faculty and speaker at the San SevoloAlumini meeting (ILAE). | 2009 | PECS, Budapest (ILAE world congress 2009) |
| 138 | Keynote speaker at the 3rd Asian Epilepsy Surgery Congress (AESC). | Jun-09 | Osaka, Japan. |
| 139 | Attended and participated as a faculty and board of Director at the world congress of International brain mapping society. | November, 2008 | www.IBMISPS.org, held in UCLA. |
| 140 | “Trend of epilepsy surgery in India” Guest lecture presented at the World congress AESC, Beijing China, | 2008 | World congress AESC, Beijing China. |
| 141 | “Epilepsy surgery in India” Guest lecture delivered at the Japanese Epilepsy society. | 2008 | Tokyo, Japan. |
| 142 | Attending International faculty and presented paper: Epilepsy surgery for post infectious pathologies; experience from AIIMS. | 2007 | Asiano-Oceanic congress, Xiamen, China, 2007 |
| 143 | North America skull base meeting: Phoenix, Arizona, USA, attended the meeting. | 2006 | Phoenix, Arizona, USA |
| 144 | Advanced Neuroendoscopy workshop at UCLA: under Prof Frazee. | Feb 2006. | UCLA. |
| 145 | “Role of MRI-SPECT coregistration and diffusion weighted images in localizing the epileptogienic tuber in tuberous sclerosis” Poster presented at the American Epilepsy association (AES). | December 2005. | Washington DC |
| 146 | 2004; “Cognitive outcome comparison between right and left temporal surgeries for intractable epilepsy” Poster presented at “15th Cleveland-Bethel advanced symposium on epilepsy management with workshop in techniques in epilepsy surgery”. | July 15-18th, 2004 | Cleveland Clinic, US. |
| 147 | 2003; “Neuropsychological assessment of patients undergoing epilepsy surgery using a customised Hindi battery” Poster presented at International epilepsy congress held at Lisbon in October 2003 Chandra PS, Sanyal S, Gupta S, Singh VP, Bhatia M, Gaikwad S, Tripathi M, Mehta VS. Neuropsychological assessment and outcome following surgery for intractable epilepsy using specially developed battery for Indian patients. Epilepsia, 25 th IEC proceedings. Epilepsia, vol 44, supp 8, 103, 2003. | Oct-03 | Lisbon |
| 148 | 2002; Attended the Annual STICH investigators meeting as one of the STICH investigators. | June 29th, 2002 | Newcastleupontyne, U.K. |
| 149 | “Traumatic CV junction anomalies: Experience of 125 cases over 10 years”. | 26th to 29th, June, 2002. | EMN congress held at Newcastle. |
| 150 | “Management of CV junction anomalies with special reference to posterior circulation strokes: Experience of 456 cases over 10 years”: CME guest lecture given. | 14th Feb, 2002. | National Neuroscience Institute, Singapore. |
| 151 | 2002; “Management of bony CV junction anomalies: Experience of 456 cases over 10 years” Paper presented. | 16th-19th Feb, 2002 | 13th Annual Meeting of North American Skull Base Society |
| 152 | “Management of bony CV junction anomalies: Experience of 456 cases over 10 years from a tertiary centre in a developing country”: Guest lecture delivered. | 7th March, 2002. | Neurosurgical grand rounds at UCSF, San Francisco. |
| 153 | "Endoscopic management of colloid cyst of third ventricle- series of 23 cases" paper presented. | November, 2002. | Asian Congress of Neurological Surgeons, Hong Kong, |
| 154 | “Role of mild hypothermia in aneurysmal surgery” Paper presented. at the International update of Clinical Neuropharmacology. | 2001 | Maldives. |
| 155 | “Craniovertebral Junction Anomalies with posterior circulation territory infarcts:A short series” :RamDas GV, Chandra PS, Kale SS- Paper presented. | 2001 | 12th World Congress of Neurosurgery, Sydney. |
| 156 | “A decade of Trans-oral surgery- Analysis of 385 patients of CV Junction anomalies: Kale SS, Chhabra RS, Chandra PS, Patir R. Paper read at | 2001 | 12th World Congress of Neurosurgery, Sydney. |
| 157 | “Cerebral meningiomatosis presenting with intractable seizures” Poster presented. | November 11-13th, 2000. | 3rd Congress of Asian Epilepsy Organisation (AOEO), New Delhi, |
| 158 | “Foramen magnum tumours: AIIMS experience”- Paper presented at the 5th Asian-oceanian International congress on skull base surgery. | Nov 12-15th 1999 | Mumbai. |
| 159 | Faculty and guest lecture: Symposium on Paediatric epilepsy surgery organized in Hyderabad by the local epilepsy society. Gave talks on [1] Invasive monitoring for epilepsy [2] Hypothalamic hamartoma | 2011; November 5-6th | Hyderabad. |
| 160 | NEUROVASCON, 2011: [1] Key hole approach to aeurysems [2] Basilar top aneurysm | 2011; October. | |
| 161 | Faculty and Guest lecture: Circumferential fusion for dorsal instability | 2011; September. | Neurospinal Surgeons association annual congress, Bangalore |
| 162 | Guest Invited lecture: Keyhole approach to aneurysms: presented. | 2010; September | NEUROVASCON 2010, Bhubneswar |
| 163 | Guest lecture at the Indian Institute of Science: Developing lab models to create better surgical paradigms for epilepsy surgery | 2010; July. | |
| 164 | Symposium on Epilepsy; Patna. Organized by Bihar Chapter of Indian Epilepsy Society; Guest faculty, gave lecture on “ Surgery for Intractable Epilepsy”. | 2010 | Bihar, India |
| 165 | Faculty UPNEUROCON; lecture on “Hemispherotomy for intractable epilepsy” | 2010; April | Fortis Noida. |
| 166 | Attended as an expert in the committee to develop “Guidelines to develop Epilepsy Education In India”; by the Indian Epilepsy Association” | 2010; April | - |
| 167 | Attended as an expert in the committee to develop MEG in India. | 2010; March | Atomic Research Commission, Kalpakam, Tamil Nadu |
| 168 | Faculty; Neurotropicon; JIPMER, Pondicherry; Gave a lecture: “Craniovertebral junction anomalies in India” | 2010; March | India |
| 169 | Faculty and Co Chairman for Symposium on Minimally invasive spine surgery and total disc replacement. | 2010; January 18th | New Delhi |
| 170 | Chairman of the course, SKELETAL, AO spine, on advanced managed for spinal trauma with hands of workshop. | 21-22nd November, 2009 | Gurgaon, New Delhi |
| 171 | Guest lecture, Trauma 2009: 360 degrees fusion for dorsal column instability. | 12-15th November, 2009 | JPN Apex trauma center, AIIMS. |
| 172 | Guest lecture as faculty: ILAE/ASEPA International workshop on Epilepsy surgery, Hemispherotomy for epilepsy surgery. | 7-8th November, 2009: | - |
| 173 | Guest lecture as faculty: ILAE/ASEPA International workshop on Epilepsy surgery, AIIMS: Future directions for epilepsy surgery in India. | 7-8th November, 2009 | AIIMS |
| 174 | Guest lecture as faculty: ILAE/ASEPA International workshop on Epilepsy surgery,: Conducted the round table discussion with IES on development of guidelines for epilepsy surgery in India. | 7-8th November, 2009 | AIIMS |
| 175 | 2009; Guest lecturer; AO Spine Principles Course, New Delhi, [1] Approach to Anterior cervical Spine [2] Outcome of Surgery for degenerative lumbar spine disease [3] Spinal Implant complications [4] Intraspinal tumors | Jul-09 | New Delhi. |
| 176 | “Pediatric Epilepsy Surgery”. CME guest lecture given on the occasion of “Pediatric neurosurgery CME”. | 30thMay, 2009. | CMC Ludhiana. |
| 177 | 2009; “Epilepsy Surgery”. CME guest lecture given on the “Epilepsy Update”. | 10th May 2009. | IES, Patna. |
| 178 | “Role of Electrocorticography in epilepsy surgery” CME guest lecture given. | 2008 | Annual conference of Neurological society of India, Pune. |
| 179 | Facutly, Instructional Course in Spine, August 7, Shila, delivered 4 lectures on CV junction, circumferential fusion. | 2008, August 7 | - |
| 180 | Faculty and speaker and panel participant; Indo-US, DBT-NIH workshop. | 2008 | Dept of Biotechnology; Ministry of Science and Technology, India, Hyderabad. |
| 181 | Faculty and panel discussant, Trauma 2008; International Conference cum Live Workshop, Indian Society of Trauma. | November 2008. | JPN Apex Trauma Center, AIIMS, New Delhi. |
| 182 | GEMIND: Guidelines for epilepsy management laid down by Indian Epilepsy Society; Committee meetings; attended as expert core committed for laying down National guidelines, | Aug-08 | - |
| 183 | Chairman, Workshop on Minimally invasive Spine Surgery. | March 2008. | Manipal Hospital, Bangalore. |
| 184 | “Neurosurgical perspectives of traumatic brain injury” Guest lecture given at the annual Indraprasthaphysiotherapatist’s conference. | 2008 | Indraprasthaphysiotherapatist’s conference |
| 185 | “Role of neurosurgeon in ICU infection” guest lecture given at the 2007 annual armed forces [R & R hospital] neurosciences update. | 2007 | R&R hospital |
| 186 | 2006; Post operative ICU infections: Invited Talk given in May 2006 at the R&R hospital annual conference | May-06 | R&R hospital |
| 187 | 2006; Invited guest lecture: “Epilepsy surgery in adults” at Current Trends in Epilepsy: an international symposium. | Nov 3-5th, 2006. | AIIMS. |
| 188 | “Endoscopic excision of colloid cysts” guest lecture given at Brain and spine endoscopic workshop held at Jaipur on 21-22nd February, 2004 and participated as a National faculty [workshop conducted by Prof M Gaab, Neurosurgery clinic, Hanover, Germany] | 2004 | Jaipur. |
| 189 | “CV junction anomalies: lessons learnt from 632 cases: guest lecture given at the National skull base conference. | December 2004. | Mumbai. |
| 190 | Attended and participated in the live AO SPINE SYMPOSIUM. | 4-6TH July, 2003. | Cochin |
| 191 | “Surgery for pediatric intractable epilepsy” Invited guest lecture given at PEDINEUROCON 2003 [National convention on Pediatric Neurology: Indian academy of Pediatrics] | November 22nd, 2003 | PEDINEUROCON 2003 |
| 192 | “Neuroendoscopy” Invited guest lecture given at the CME section of the Neurological Society of India, PGI Chandigarh in “How I do it?” | 12thDecemebr, 2003. | Neurological Society of India, PGI Chandigarh. |
| 193 | “Neuroendoscopy” guest lecture given on the CME: How I do It? Of the Neurological Society of India annual conference held in PGI, Chadigarh, | Decemebr 2003. | PGI, Chadigarh. |
| 194 | “Epilepsy surgery for pediatric patients: AIIMS experience” guest lecture given at Pedineurocon 2203. | 22ndNovemeber 2003. | Jaipur. |
| 195 | “Trans oral surgery for CV junction anomalies & Odontoid screw fixation for type II dens fracture: How I do it?” Video sessions of personally operated cases shown as an invited guest speaker at SPINE 2002. | 18th-21st July, 2002. | Kanyakumari. |
| 196 | “CV junction anomalies: Experience of single stage surgery from 516 cases”. Talk given as an invited guest speaker at SPINE 2002. | 18th-21st July 2002. | Kanyakumari. |
| 197 | 2002; "Management of head injuries" Invited lecture given for CME on 'Management of a trauma patient'. | December 22, 2002. | Association of surgeons of India- ASICON CME education foundation, New Delhi. |
| 198 | “Head injuries- Recent trends in Management”- Talk given on the inaugural function of the 2nd Nursing update held in the Nursing College All India Institute of Medical sciences. | 2001 | AIIMS. |
| 199 | 2001; Participitated as a panellist on one-day symposium on “Modern day concepts in disinfection &sterilisation practices”. | 17th February 2001. | AIIMS. |
| 200 | 2001; Gave a talk on “Aseptic practices in clinical practice” as an invited speaker on the occasion of National conference on infection control in India hospitals, was the chairperson of one of the groups in the workshop for setting the “National policy for guidelines on aseptic practices, disinfection and sterilization procedures”. | OCT 17-19, 2001. | AIIMS. |
| 201 | Endoscopic management of colloid cysts: Series of 18 cases:Ramdas GV, Suri A, Chandra PS; Paper read at NEUROCON 2001. | 2001 | Neurological Society of India, Mumbai. |
| 202 | ; “Posterior circulation strokes associated with cranio-vertebral junction anomalies: Series of 9 cases”: Paper presented at NEUROCON 2001. | 2001 | Neurological Society of India, Mumbai. |
| 203 | ; “Endoscopic management of the cystic lesions of brain” Talk given as one of the guest speakers at the Minimal access neurological surgery workshop,chaired by Prof Pernezky 2001. | Feb 23-24th, 2001. | Sir Ganga Ram hospital. |
| 204 | “Endoscopic evacuation of spontaneous intracerebral hematomas”: Guest lecture presented on the occasion of 3rd Annual meeting of Delhi Neurological Association, 2001. | 2001 | Annual meeting of Delhi Neurological Association, 2001. |
| 205 | 2001; “Craniovertebral junction anomalies: A retrospective study of 385 cases- lessons learnt”- Paper presented at the National conference of Spine. | July 2001. | Kodaikanal. |
| 206 | “Craniovertebral junction anomalies : Lessons learnt in 10 years”: Paper read at 3rd National skull base conference, Madras, 2001. | 2001 | National skull base conference, Madras. |
| 207 | “Trigeminal neurinomas: A series of 25 cases” paper presented at SGPGI, skull base conference. | 2000 | Post graduate Institute, Lucknow. |
| 208 | “Trigeminal neurinomas: A series of 25 cases” paper presented at SGPGI, skull base conference. | 2000 | Post graduate Institute, Lucknow. |
| 209 | Attended and actively participated the Midas Rex hands on workshop. | Mar-99 | AIIMS. |
| 210 | “Post traumatic epilepsy” Talk given on the occasion of the inaugural function of Delhi Neurological Association held at Sir Ganga Ram Hospital in April’ 99 and participated as one of the members in the panel discussion. | Apr-99 | Sir Ganga Ram Hospital |
| 211 | 1999; “Hands on workshop on Neuroendoscopy” Participated this workshop.(conducted by A Pernezky, T Kanno, Y,. Kato, AK Banerjii). | Nov 10-12th, 1999. | VIMHANS |
| 212 | 1999; “Hands on workshop on neuroendoscopy and Neuronavigation” Participated this workshop (conducted by M. Gaab, A Grotenhuis, Hechl P) | Sept 9th, 1999. | CMC Vellore |
| 213 | “Paediatric nosocomial infections in neurosurgery” Paper presented at the International Paediatric CME held at Calcutta, | Dec 1998. | International Paediatric CME held at Calcutta, |
| 214 | “Cavernous sinus neurofibromas arising from ocular cranial nerves” Paper presented at the First National skull base conference. | Nov, 1998. | New Delhi. |
| 215 | “Hands on workshop on spinal surgery” Participated this workshop. | June 21-22nd, 1997. | MS Ramaiah Medical college. |
| 216 | “Neuroendoscopic management of unilateral hydrocephalus” Poster presented at NSI Calcutta-96. | 1996 | NSI Calcutta-96. |
| 217 | 1994;“CME on Pediatric Neurosurgery” attended this CME held at Mumbai (conducted by Marion L Walker and SN Bhagawati). | March 12-16th, 1994. | Mumbai. |
| 218 | “Morbidity and Mortality in surgery for pituitary adenomas” Paper presented at Neurological society of India, Madras 1993. | 1993 | Madras. |
DETAILS OF RESEARCH WORK
Dr P Sarat Chandra is currently working as Professor and Head of Unit I at the Dept of Neurosurgery, AIIMS, Delhi. He is the Team Leader for Centre of Excellence for Epilepsy (COE) and the faculty in charge for the Epilepsy Surgery and Functional Neurosurgery Fellowship Program in AIIMS.
- Publications & Papers presented in International & National Conferences: Till date, he has published over 462 papers (h index of 37 and total citations of over 4712; (https://scholar.google.com/citations?user=C_fTZQsAAAAJ&hl=en), gave over 150 guest lectures (India and Abroad) and has also conducted several live surgery workshops (India and Abroad). His papers include some of the highest impact papers which include NEJM, Genomics, Epilepsia, Scientific Reports (Nature), Neurosurgery, Journal of Neurosurgery, The Spine Journal, and Epilepsy Research to mention few. He was chief surgeon in the first ever randomized study for the study “Surgery for Drug Resistant Epilepsy in Children” published as an original paper in New England Journal of Medicine (was ranked as the top ten papers of 2018 in NEJM)[1, 2]. [3-54]. He is currently the Chief Editor of Neurology India (Impact factor 2.71). He has been the chief guide to over 10 PhD students, and over 25 MCh candidates for their dissertations.
- Affiliations to Journals:
- Editor in Chief for Neurology India (Impact factor 2.1): This is the oldest (60 years) and the most prestigious journal for Neurosurgery, Neurology and allied Neurosciences in India.
- Reviewer: He is the reviewer of several journals including Scientific Reports- Nature, Epilepsia, Neurosurgery, World Neurosurgery, Epilepsy Research, The Spine Journal and Journal of Neurosurgery to mention a few
- Affiliations to various Scientific Bodies: He is the executive member and occupies leadership positions in several National and International Scientific bodies and Societies (International League Against Epilepsy-ILAE- In Charge of Developing Countries; Asian Epilepsy Surgery Society- Past President & Executive, Asiano-Oceanic Commission for Epilepsy-Co-Chair Epilepsy Surgery, Indian Epilepsy Society- Executive member; Skull base Society of India- President Elect and past secretary, Cerebrovascular Society of India- Secretary, Neuro-endoscopic Society of India-Treasurer). He has been also elected as a member for the prestigious National Science Academy (FNASc) of India.
- Extra-mural Research Grants:
- He has been the PI and Co-PI of several Research Grants (funded by DBT, DST and various other extramural projects). Of important, to mention is the [1.] PI for development of Centre of Excellence for Epilepsy and MEG, which is a collaborative project between AIIMS & NBRC. The project has been sanctioned in 2012 and has done significant work in developing newer surgical techniques, finding novel mechanisms for epileptogenesis and networks and has patents for new molecules and surgical techniques. The centre has published over 65 high impact papers and has conducted over 5 workshops and trained several PhD students and fellows for Neurosurgery (4 including one from Indonesia) and Neurology (3). The COE has recently got its Phase II [2.]
- PI for Research grant from the office of Principle Scientific Advisor to PM office (Govt to India) on developing Advance research methodologies for Epilepsy. This includes developing for the first time a portable video EEG system with an AI interface (along with IIT, Delhi) along with 3 other research project to identify novel molecular drug mechanisms and newer drugs.
- Patents and Intellectual Property Rights: He has over 7 patents, including 1 patent with USA and PCT (Paris Convention Treaty) International patent. He has developed new surgical techniques for the first time which have been validated and published. These include 1.] Endoscopic Hemispherotomy for epilepsy: a minimally invasive procedure to disconnect whole single procedure[23, 30, 55-57], 2.] Endoscopic corpus callosotomy for epilepsy: a minimally invasive procedure to treat severe drug resistant epilepsy 3.] Radiofrequency ablation disconnection of hypothalamic hamartoma using Robotic and O-arm guidance: a minimally invasive technique for these challenging lesions[6]. 4.] DCER- A new technique to treat severe atlanto axial dislocation and basilar invagination [58-65].5.] Endoscopic disposable carpal tunnel set.
- His other specific contributions include
- He is also developing for the first time a portable Video EEG device with smart phone interface along with AI component along with IIT Delhi, with funding from PSA office (Principle Scientific Advisor’s office to Govt of India).- Figure 7
- Developing a new innovative technique for cranio-vertebral junction anomaly (DCER) which has been validated and published in high impact research papers (Neurosurgery IF 4.2; Neurology India: 2.7). This technique has cut down the time of surgery to < 50% and has also reduced the morbidity by > 50%. This has also led the author to develop new implants (with funding from DBT, Ministry of Science & Technology) and a new type of Universal CVJ reducer (as a research collaboration with R&D division of Medtronics, USA. Medtronics is the leading company for spine innovation and the nominee is the first person to do this kind of collaboration.)- Figure 8
- Developed the technique of Alcohol embolization and short segment fixation of vertebral haemangiomas, which has made surgery for this kind dangerous pathologies very easy and safe with excellent long term results. This has been validated and published as 3 papers (Neurosurgery, IF:4.2; Child’s nervous system, IF:3.7 and The Spine Journal; IF: 3.8).- Figure 9
- Developed and patented a special endoscopic retractor for performing pituitary surgeries endoscopically. The retractor is unique, made of a special alloy, coated with non-stick Teflon and fibrin and makes pituitary surgeries safer, easier and more effective.- Figure 10
- Summarizing his primary area of focus has been Epilepsy, Epilepsy surgery and epilepsy networks where he has contributed significantly providing new surgical techniques, understanding mechanisms of epileptogenesis and epilepsy networks and also provide and create research and training facilities to take this further. He has created a centre of Excellence for Epilepsy & MEG centre (AIIMS & National Brain Research Centre).
- Apart from this, He has also contributed in spine (cranio-vertebral junction and Vertebral body hemangiomas) by creating new surgical techniques, patenting new instruments and implants which have made the surgery easier, safer, and with less morbidity.
- Over his career of over 20 years, he has trainedseveral students and PhD’s (>35) and has operated over 25,000 surgeries.
Research Projects (Tabular Summary): Total Funding for all research projects: 52 crores (approx.)
| Project No. | Grant | Research proposed | Research outcome |
|---|---|---|---|
| 1. | Principal Scientific Advisor, (PSA), Govt of India | Development and demonstration of a portable device for rapid detection of epileptiform discharges | Portable device development for rapid detection of epileptiform discharges in low cost clinical settings |
| Investigating the role of dysfunctional benzodiazepine binding site on GABA A receptor in benzodiazepine resistance associated with drug resistant epilepsy | Benzodiazepine resistance is caused by alterations in expression levels of GABA A receptor subunits in DRE | ||
| Investigating the role of mass spectrometric lipid profiles of brain tissues resected from patients with focal cortical dysplasia in defining the epileptogenic zone | Epileptogenic zone of Graded tissue of FCD is being demarcated by using the expression of lipids in those regions as biomarkers. | ||
epilepsy research i)molecular modelling to understand resistance to anti epileptic drug ii)identification of novel drug targets using tools of data science | Development of resistance in DRE by molecular modelling of drug targets using bioinformatics tools | ||
| 2. | COE Phase II, DBT, Govt of India | Eloquent cortex mapping in chronic intractable epilepsy using Nex-Stim Navigated brain stimulation system (NBS), functional MRI and MEG: A comparative study. | Accurate localisation of epileptogenic zone by various imaging techniques leads to better management of seizures |
| Investigating the role of metabolites and neurotransmitters in abnormal synaptic transmission associated with mesial temporal lobe epilepsy (MTLE) and focal cortical dysplasia (FCD): Possible biomarkers for localization of epileptogenic foci. | Alterations in the frequency and amplitude of EPSPs after kyunurenic acid application Alterations in levels of glutamate and GABA neurotransmitters in DRE leading to hyper excitability | ||
| Validation of the potential candidate genes identified in both MTLE and FCD patients for their possible role as prognostic/diagnostic biomarkers. | Various genes like FN1, TGFbeta, SMAD3, MMP9 are found to be altered in DRE patients and can be used as potential diagosnitic biomarkers | ||
| 3. | SERB, DST, Govt. Of India | Deciphering the role of casein kinase 2 in mesial temporal lobe epilepsy | Alterations in CK2 levels in MTLE contribute to hyperexcitability associated with MTLE |
| 4. | DBT, Govt of India | Role of kynurenic acid, a glutamate receptor inhibitor, in hyper excitability associated with mesial temporal lobe epilepsy | Reduced kynurenic acid relates to alterations in hyperexcitability in mesial temporal lobe epilepsy |
Complete list of books, monographs etc. published.
- “Evolution of Neurosurgical techniques” Tandon and Ramamurthi's Textbook of operative Neurosurgery.
- “History of Microneurosurgery” Tandon and Ramamurthi's Textbook of operative Neurosurgery.
- Banerji AK, Mehta VS, Chandra PS. - Transsphenoidal surgery for sellar and suprasellar tumours – Tandon and Ramamurthi's Textbook of operative Neurosurgery.
- Chandra PS, Hegde T(1998)Neurosurgery of psychiatric disorders. Advances in Clinical Neurosciences (Annual CME book of Association of Neuroscientists of Eastern India).
- Chandra PS, Mahapatra AK. Improving outcome in head injuries- In Mahapatra AK (ed).A textbook of Head injury- 1999 (Modern publishers) - 2nd edition.
- Chandra PS, Mahapatra AK. Prevention of Head injuries- In Mahapatra AK (ed).A textbook of Head injury- 1999 (Modern publishers), pp 262-267.
- Chandra PS, Mahapatra AK. Role of calcium ions in Head injuries- In Mahapatra AK (ed).A textbook of Head injury- 1999 (Modern publishers) - 2nd edition. In press.
- Chandra PS, Mahapatra AK. Traumatic basal ganglonic hematomas- In Mahapatra AK (ed).A textbook of Head injury- 1999 (Modern publishers) - 2nd edition. In press.
- Chandra PS, Mehta VS, Aggarwal SP. Head injuries and psychiatric disturbances. In Mental Health: An Indian perspective- 146-2003 ed: Aggarwal SP, Goel DS Directorate General of health services, Ministry of health and Family welfare, New Delhi: Elsevier. Pp306-312
- Chandra PS, Mehta VS. Aseptic practices in Medical and Surgical practice: chapter for Manual on disinfection, sterilization and aseptic practices in Medicine and Surgery. In press.
- Chandra PS, Mehta VS. Entrapment Neuropathy. Indian Textbook of Neurosurgery. Ed Ramamurthi and Tandon, 2010
- Chandra PS, Mehta VS. Neuroendoscopy: Chapter written in the CME book for the NSI annual conference, 2003
- Chandra PS, Sharma BS. Fifth Nerve Schwanommas. Indian Textbook of Neurosurgery. Ed Ramamurthi and Tandon, 2010.
- Chandra PS, Tandon PN. Brain tumors. API textbook, 2011
- Chandra PS, Tandon V. AIDS and the Neurosurgeon. Indian Textbook of Neurosurgery. Ed Ramamurthi and Tandon, 2010
- Chandra PS, Tripathi Manjari, Surgery for Intractable Epilepsy. In Epilepsy Review ed Ashok Kumar, Jaypee publications.
- Chandra PS, Tripathi Manjari. Epilepsy Surgery; Guidelines. CME book on Update on Epilepsy surgery, [Indian Epilepsy Society] held at Patna, May 10th, 2009.
- Chandra PS, Tripathi Manjari. Role of Electrocorticography in epilepsy surgery, 2008, CME book for NeuroCon 2008, NSI, Pune.
- Chandra PS, Chandramouli BA (1997).Cervical orthosis and traction Chapter for the monogram Craniovertebral junction anomalies- Indian experience published on the occasion of the 1st CV junction conference held at SGPGI Lucknow in October, 97.
- Chandra PS. Traumatic abnormalities of the CV junction. Indian Textbook of Neurosurgery. Ed Ramamurthi and Tandon, 2010.
- GEMIND: Guidelines for epilepsy management in India; Contributed towards this book published by the Indian Epilepsy Society.
- Hegde T, Chandra PS (1998) Neurosurgery of movement disorders.Advances in Clinical Neurosciences (Annual CME book of Association of Neuroscientists of Eastern India).
- Mehta VS, Chandra PS. - Preoperative evaluation of neurosurgical patients- Chapter for the textbook of operative neurosurgery by Tandon and Ramamurthi.
- Mehta VS, Chandra PS. - Surgical procedures for cerebral revascularisation and stroke. In Bansal BC, Aggarwal AK (eds); Recent concepts in stroke (Indian college of physicians, AAPI), 1999 pp235-246.
- Mehta VS, Chandra PS. Entrapment neuropathy: In Ramamurthi B, Tandon PN, Textbook of Neurosurgery 3rd edition:
- Mehta VS, Chandra PS. Pediatric brain tumours. In Gupta AK (ed), Textbook of Pediatric Surgery (Indian Association of Pediatric Surgeons), 2001.
- Mehta VS, Chandra PS. Rhizotomies and peripheral neurectomies as pain relief surgical procedures- Chapter for the textbook of operative neurosurgery by Tandon and Ramamurthi.
- Mehta VS, Chandra PS. Surgical management of brainstem tumours: From a conservative view to a radical approach. Progress in clinical Neurosciences, 2001.
- Mehta VS, Chandra PS. Surgical management of brainstem tumours. Indian edition of Clinical neurosurgery, 2001
- Mehta VS, Chandra PS. Traumatic nerve injuries. In Mohandas S, Borgohain R, Meena AK (eds), Reviews in Neurology (IAN), 1999, pp138-147.
- Sharma BS, Chandra PS. Neurocysticercosis: Surgical Aspects. In Prabhakar S, Gagandeep Singh (eds). Neurocysticercosis.
- Sharma BS, Chandra PS. Neurocysticercosis. In Ramamurthi B, Tandon PN, Textbook of Neurosurgery 3rd edition.
- Tripathi M, Chandra PS. Electrodiagnosis in Neurosurgery. Indian Textbook of Neurosurgery. Ed Ramamurthi and Tandon, 2010
- Text books: Brain haemorrhage:Chandra PS, Mahapatra AK. Jaypee publication
- AIIMS operative atlas of operative neurosurgery: in publication: Wolters Kluwer
- *Endoscopic assisted hemispherotomy: Chandra PS et al, In Pediatric Epilepsy Surgery (Oguz Cataltepe, George I Jallo, Second Edition, Thieme publications, 2019
- *Endoscopic assisted corpus callosotomy with commissurotomy: Chandra PS et al, In Pediatric Epilepsy Surgery (Oguz Cataltepe, George I Jallo, Second Edition, Thieme publications, 2019
- *Endoscopic assisted hemispherotomy, Chandra PS et al, In Operative technique in Epilepsy Surgeyr (Gordon Baltuch, Arthur Cukiert), Thieme publications, 2019
*Chapters as shown in list above and also as a screen shot are the techniques developed by the author for the first time in literature and now accepted worldwide and also standard chapters in textbooks. The above 2 textbooks are highly reputed textbooks in this field.
ALL PUBLICATIONS
- Agarwal, S., Sharma, M.C., Singh, G., Suri, V., Sarkar, C., Garg, A., Kumar, R., and Chandra, P.S. (2012). Papillary glioneuronal tumor—a rare entity: report of four cases and brief review of literature. Child's Nervous System 28, 1897-1904.
- Agrawal, D., Chandra, P., Singh, P., Meena, R., Doddamani, R., Jagdevan, A., Mishra, S., and Garg, K. (2020). Cost-Effective Home Mechanical Ventilation in Neurosurgery Patients: Case Series of Three Patients. Journal of neurosciences in rural practice 11, 329.
- Agrawal, M., Chandra, P.S., Doddamani, R., Kaur, K., Samala, R., and Tripathi, M. (2020). Maximizing non-invasive investigations in the quest for identifying the epileptogenic zone. Clinical neurophysiology: official journal of the International Federation of Clinical Neurophysiology 131, 2777-2778.
- Agrawal, M., Dharanipathy, S., Nakra, T., Garg, K., Gurjar, H., Mishra, S., Singh, M., and Chandra, P.S. (2019). Supratentorial Neurenteric Cyst: A Rare Differential for a Frontal Cyst. World neurosurgery 129, 140-142.
- Agrawal, M., Garg, K., Mishra, S., Doddamani, R., and Chandra, P.S. (2020). Letter to the editor regarding “Selective dorsal rhizotomy for spasticity of genetic etiology”. Child's Nervous System 36, 1825-1825.
- Agrawal, M., Garg, M., Kumar, A., Singh, P.K., Satyarthee, G.D., Agrawal, D., Chandra, P.S., and Kale, S.S. (2018). Management of pediatric posttraumatic thoracolumbar vertebral body burst fractures by use of single-stage posterior transpedicular approach. World neurosurgery 117, e22-e33.
- Agrawal, M., Samala, R., Doddamani, R., Agrawal, D., and Chandra, S.P. (2020). The role of selective dorsal rhizotomy in the management of post-traumatic spasticity: systematic review. Neurosurgical review, 1-9.
- Agrawal, M., Samala, R., Doddamani, R.S., Goyal, A., Tripathi, M., and Chandra, P.S. (2021). Is surgery effective for treating hypothalamic hamartoma causing isolated central precocious puberty? A systematic review. Neurosurgical Review, 1-19.
- Agrawal, M., Sawarkar, D., Singh, P.K., Mishra, S., Meena, R., Gupta, D.K., Chandra, P.S., and Kale, S.S. (2021). Posterior fixation for paediatric and adolescent unstable hangman’s fracture: evolution to C1 sparing techniques. Child's Nervous System, 1-9.
- Agrawal, M., Tripathi, M., Samala, R., Doddamani, R., Ramanujan, B., and Chandra, P.S. (2021). Epilepsy surgery in COVID times—a unique conundrum. Child's Nervous System, 1-6.
- Ahmad, F.U., Chandra, P.S., Sanyal, S., Garg, A., and Mehta, V.S. (2005). Sellar tuberculoma: An unusual infection. Indian Journal of Tuberculosis 52, 215.
- Ahmad, F.U., Sharma, B.S., Garg, A., and Chandra, P.S. (2008). Primary spontaneous CSF rhinorrhea through the clivus: possible etiopathology. Journal of Clinical Neuroscience 15, 1304-1308.
- Ahmad, F.U., Tripathi, M., Padma, M., Gaikwad, S., Gupta, A., Bal, C., Sarkar, C., Gupta, S., Wadhawan, A.N., and Sharma, B.S. (2007). Health-related quality of life using QOLIE-31: before and after epilepsy surgery a prospective study at a tertiary care center. Neurology India 55, 343.
- Ailawadhi, P., Chandra, P.S., Sharma, M., and Mahapatra, A. (2012). Central liponeurocytoma: Case report and review of literature. Indian Journal of Neurosurgery 1, 083-085.
- Amitkumar, M., Singh, P.K., Singh, K.J., Khumukcham, T., Sawarkar, D.P., Chandra, S.P., and Kale, S.S. (2020). Surgical Outcome in Spinal Operation in Patients Aged 70 Years and Above. Neurology India 68, 45.
- Ammini, A.C., Bhattacharya, S., Sahoo, J.P., Philip, J., Tandon, N., Goswami, R., Jyotsna, V.P., Khadgawat, R., Chumber, S., and Seth, A. (2011). Cushing’s disease: results of treatment and factors affecting outcome. Hormones 10, 222-229.
- Amsden, B., Chen, F., Hochleitner, G., Groll, J., Dalton, P., Jüngst, T., Hrynevich, A., Brook, G., Groll, J., and Dalton, P. (2015). 2015 4th TERMIS World Congress Boston, Massachusetts September 8–11, 2015. Tissue Engineering Part A 21, S-1-S-413.
- Andersson, D., Boehme, B., Chandra, C., Chen, S., Frisk, L., Gutierrez, M., Hajizadeh, A., Hansson, J., Hassona, A., and Helminen, E. Author List.
- Bahl, V., Chandra, S., and Yadav, R. (1997). Percutaneous transvenous balloon aortic valvuloplasty by antegrade transseptal approach using Inoue balloon catheter.
- Bajaj, J., and Chandra, P.S. (2020). Recent Developments in Endoscopic Endonasal Approach for Pituitary Adenomas. Neurology India 68, 79.
- Bajaj, J., Chandra, P.S., Ramanujam, B., Girishan, S., Doddamani, R., and Tripathi, M. (2018). Hemispherotomy in Adults. Is It Safe?—A Prospective Observational Study in Comparison to Children. International Journal of Epilepsy 5, A0018.
- Bajaj, J., Chandra, S.P., Ramanujam, B., Girishan, S., Doddamani, R., and Tripathi, M. (2019). Need of Immediate Drug Reduction after Epilepsy Surgery–A Prospective Observational Study. Neurology India 67, 1050.
- Bajaj, J., Chaudhary, K., Chandra, P.S., Ramanujam, B., Girishan, S., Doddamani, R., Tripathi, M., Nehra, A., and Tripathi, M. (2020). Left temporal lobectomy using functional MRI in a math genius: A case report. Neurology India 68, 170.
- Bajaj, J., Tripathi, M., Dwivedi, R., Sapra, S., Gulati, S., Garg, A., Tripathi, M., Bal, C.S., and Chandra, S.P. (2018). Does surgery help in reducing stigma associated with drug refractory epilepsy in children? Epilepsy & Behavior 80, 197-201.
- Banerjee, J., BanerjeeDixit, A., Srivastava, A., Ramanujam, B., Kakkar, A., Sarkar, C., Tripathi, M., and Chandra, P.S. (2017). Altered glutamatergic tone reveals two distinct resting state networks at the cellular level in hippocampal sclerosis. Scientific reports 7, 1-13.
- Banerjee, J., Chandra, S.P., Kurwale, N., and Tripathi, M. (2014). Epileptogenic networks and drug-resistant epilepsy: Present and future perspectives of epilepsy research-Utility for the epileptologist and the epilepsy surgeon. Annals of Indian Academy of Neurology 17, S134.
- Banerjee, J., Dey, S., Dixit, A.B., Doddamani, R., Sharma, M.C., Garg, A., Chandra, P.S., and Tripathi, M. (2020). GABAA Receptor-Mediated Epileptogenicity in Focal Cortical Dysplasia (FCD) Depends on Age at Epilepsy Onset. Frontiers in cellular neuroscience 14.
- Banerjee, J., Dey, S., Dixit, A.B., Tripathi, M., Doddamani, R., Sharma, M.C., and Chandra, P.S. (2020). α7 nicotinic receptors contributes to glutamatergic activity in the hippocampus of patients with mesial temporal lobe epilepsy with hippocampal sclerosis (MTLE-HS). Journal of Neural Transmission 127, 1441-1446.
- Banerjee, J., Dixit, A.B., Tripathi, M., and Chandra, P.S. (2016). Endogenous activity of NMDA receptors contributes to the enhanced glutamatergic tone and hyperexcitability in resected brain samples obtained for patients with mesial temporal lobe epilepsy. International Journal of Epilepsy 3, A28.
- Banerjee, J., Dixit, A.B., Tripathi, M., Sarkar, C., Gupta, Y.K., and Chandra, P.S. (2015). Enhanced endogenous activation of NMDA receptors in pyramidal neurons of hippocampal tissues from patients with mesial temporal lobe epilepsy: A mechanism of hyper excitation. Epilepsy research 117, 11-16.
- Banerjee, J., Tripathi, M., and Chandra, P.S. (2013). Understanding complexities of synaptic transmission in medically intractable seizures: A paradigm of epilepsy research. Indian J Neurosurg 2, 71-76.
- Banerjee, J., Tripathi, M., Chandra, P.S., and Dixit, A.B. (2020). Do SARS-CoV2 viral proteins have neuromodulatory properties? Neurology India 68, 274.
- Bansal, S., Ailawadhi, P., Suri, A., Kale, S.S., Chandra, P.S., Singh, M., Kumar, R., Sharma, B.S., Mahapatra, A.K., and Sharma, M.C. (2013). Ten years’ experience in the management of spinal intramedullary tumors in a single institution. Journal of Clinical Neuroscience 20, 292-298.
- Baumgartner, J.E., Blount, J.P., Blauwblomme, T., and Chandra, P.S. (2017). Technical descriptions of four hemispherectomy approaches: From the Pediatric Epilepsy Surgery Meeting at Gothenburg 2014. Epilepsia 58, 46-55.
- Bharti, K., Vibhin, V., Ramanujam, B., Chandra, P.S., Ajay, G., Madhavi, T., Chandrashekar, B., and Tripathi, M. (2016). Ictal MEG yield in patients with drug refractory epilepsy undergoing magnetoencephalography. International Journal of Epilepsy 3, A29.
- Bhattacharya, K., Paul, B., and Purkayastha, S. (2020). A Case of Idiopathic Intracranial Hypertension with Bilateral Transverse Sinus Stenosis Treated with Balloon Angioplasty. Neurology India 68, 504.
- BIndira, D., Chandra, S., Mongia, S., Chandramouli, B., Sastry, K., and Shankar, S. (2002). Spinal intramedullary tuberculoma and abscess: a rare cause of paraparesis. Neurology India 50, 494.
- Bindra, A., Chouhan, R.S., Prabhakar, H., Chandra, P.S., and Tripathi, M. (2015). Perioperative anesthetic implications of epilepsy surgery: a retrospective analysis. Journal of anesthesia 29, 229-234.
- Bindra, A., Chouhan, R.S., Prabhakar, H., Dash, H.H., Chandra, P.S., and Tripathi, M. (2012). Comparison of the effects of different anesthetic techniques on electrocorticography in patients undergoing epilepsy surgery–A bispectral index guided study. Seizure 21, 501-507.
- Bindra, A., Kaushal, A., Prabhakar, H., Chaturvedi, A., Chandra, P.S., Tripathi, M., Subbiah, V., Sathianathan, S., Banerjee, J., and Prakash, C. (2019). Neuroprotective role of dexmedetomidine in epilepsy surgery: A preliminary study. Neurology India 67, 163.
- Bir, M., Gupta, U., Jaryal, A.K., Singh, A., Netam, R., Kale, S.S., Chandra, S.P., Singh, M., and Rath, G.P. (2021). Predictive value of intraoperative D-wave and m-MEP neurophysiological monitoring in patients with preoperative motor deficits in immediate and late postoperative period. Journal of Craniovertebral Junction & Spine 12, 26.
- Bisht, A., Suri, A., Bansal, S., Chandra, P.S., Kumar, R., Singh, M., and Sharma, B.S. (2014). Factors affecting surgical outcome of endoscopic third ventriculostomy in congenital hydrocephalus. Journal of Clinical Neuroscience 21, 1483-1489.
- Bohara, S., Garg, K., Mishra, S., Tandon, V., Chandra, P.S., and Kale, S.S. (2021). Impact of various cervical surgical interventions in patients with Hirayama’s disease—a narrative review and meta-analysis. Neurosurgical Review, 1-19.
- Bora, S., Kumar, A., Mishra, S., Satyarthee, G.D., Singh, P.K., Sawarkar, D., Verma, S., Borkar, S., Sharma, R., and Chandra, S.P. (2019). Intracranial aspergillosis amongst immunocompetent patients: An experience with combined surgical and medical management of 18 patients. Clinical neurology and neurosurgery 186, 105511.
- Bora, S.K., Suri, A., Khadgawat, R., Tandon, N., Suri, V., Sharma, M.C., Satyarthee, G., Singh, M., Tandon, V., and Agarwal, D. (2020). Management of Cushing's disease: Changing trend from microscopic to endoscopic surgery. World neurosurgery 134, e46-e54.
- Borkar, S.A., Singh, M., Kale, S.S., Suri, A., Chandra, P.S., Kumar, R., Sharma, B.S., Gaikwad, S., and Mahapatra, A.K. (2018). Spinal cerebrospinal fluid drainage for prevention of vasospasm in aneurysmal subarachnoid hemorrhage: A prospective, randomized controlled study. Asian journal of neurosurgery 13, 238.
- Chandra, P. (2020). Plasma Technologies for Health Applications. Neurology India 68, 3-4.
- Chandra, P. (2020). Telemedicine: The Next Important Health Vertical for Neurosciences In India. Neurology India 68, 532-532.
- Chandra, P., Bal, C., Garg, A., Gaikwad, S., Prasad, K., Sharma, B.S., Sarkar, C., Singh, M., Padma, V.M., and Tripathi, M. (2010). Surgery for medically intractable epilepsy due to postinfectious etiologies. Epilepsia 51, 1097-1100.
- Chandra, P., and Dash, H. (2011). Absolute Ethanol Embolization With Instrumented Fusion Is Very Effective But May Be Used With Caution. Neurosurgery.
- Chandra, P., and Dave, P. (1970). Effect of dipyrone on tourniquet shock. Arzneimittel-forschung 20, 409-413.
- Chandra, P., Dave, P., and Vasudeo, N. (1970). Effect of Phenoxybenzamine on Lactate and Pyruvate Levels in Tourniquet Shock. The Indian journal of medical research 58, 230-233.
- Chandra, P., and Hegde, T. (2000). A case of coexisting cerebellopontine angle meningioma and schwannoma. Neurology India 48, 198.
- Chandra, P., Kumar, A., Chauhan, A., Ansari, A., Mishra, N., and Sharma, B. (2013). Concepts, Innovations and Techniques Distraction, Compression, and Extension Reduction of Basilar Invagination and Atlantoaxial Dislocation: A Novel Pilot Technique. NEUROSURGERY-BALTIMORE THEN HAGERSTOWN MD- 72, 1040-1053.
- Chandra, P., and Mahapatra, A. (2001). Giant ocular nerve neurofibroma of the cavernous sinus: a series of 5 cases. Neurology India 49, 166.
- Chandra, P., Manjari, T., Devi, B., Chandramouli, B., Srikanth, S., and Shankar, S. (2000). Intramedullary spinal epidermoid cyst. Neurology India 48, 75.
- CHANDRA, P., and MANOCHA, J. (1968). certain important features of the syndrome in the light of our own observations in one. Indian Journal of Orthopaedics 2, 12.
- Chandra, P., Manocha, J., and Dave, P. (1968). Achondroplasia with paraplegia. Indian J Orthop 2, 12-23.
- CHANDRA, P., MANOCHA, J., and DAVE, P. (1968). pre-albumin, albumin, alpha, beta and gamma-globulins were isolated from human, calf, rat. Indian Journal of Orthopaedics 2, 97.
- Chandra, P., Mehta, V., Singh, V., Chaturvedi, A., Bithal, P., and Dash, H. (2004). A randomized controlled study on use of mild hypothermia for brain protection during intracranialaneurysm surgery. Journal of Neurochemistry 88.
- Chandra, P., Mukherjee, S., Deepak, K., and Tripathi, M. (2004). A comparison of autonomic functions before and after epilepsy surgery: SC111. European Journal of Neurology Supplement 11.
- Chandra, P., Padma, V., Shailesh, G., Chandreshekar, B., Sarkar, C., and Tripathi, M. (2009). Hemispherotomy for intractable epilepsy (vol 56, pg 127, 2008). NEUROLOGY INDIA 57, 49-49.
- Chandra, P., and Sabai, T. (1996). Neurocysticercosis. Journal of the Indian Medical Association 94, 82-82.
- Chandra, P., Salamon, N., and Nguyen, S. Infantile spasm-associated microencephaly in tuberous sclerosis complex and cortical dysplasia. Neurology.[Internet]. 2007 [Citado 20 de mayo de 2011]; 68 (6):[Aprox. 7p.]. In. (
- Chandra, P., Salamon, N., Nguyen, S., Chang, J., Huynh, M., Cepeda, C., Leite, J., Neder, L., Koh, S., and Vinters, H. (2007). Infantile spasm–associated microencephaly in tuberous sclerosis complex and cortical dysplasia. Neurology 68, 438-445.
- Chandra, P., Srivastava, D., and Srivastava, A. (2004). Effects of GOAW Effluents on Certain Haematological Parameters of a Catfish, Heteropneustes Fossilis(Bloch). Journal of Ecophysiology and Occupational Health 4, 197-200.
- Chandra, P., Thapa, A., Tripathi, M., Sharma, B., and Sharma, M. (2009). PO18-WE-07 Epidemiological study of post traumatic seizure in India. Journal of the Neurological Sciences 285, S245-S246.
- Chandra, P., Vaghania, G., Bal, C.S., Tripathi, M., Kuruwale, N., Arora, A., Garg, A., Sarkar, C., Diwedi, R., and Malviya, S. (2014). Role of concordance between ictal-subtracted SPECT and PET in predicting long-term outcomes after epilepsy surgery. Epilepsy research 108, 1782-1789.
- Chandra, P.S. (2012). The need for developing comprehensive epilepsy surgery units in India. Indian Journal of Neurosurgery 1, 001-003.
- Chandra, P.S. (2012). Irreducible basilar invagination and atlanto-axial dislocation: Are they really “irreducible”? Indian Journal of Neurosurgery 1, 101-104.
- Chandra, P.S. (2012). IiZ3 Improving Outcome after Traumatic Brain Injury. Textbook of Traumatic Brain Injury, 143.
- Chandra, P.S. (2013). The changing trends in management of spinal tuberculosis: Are we hitting a better road? Indian Journal of Neurosurgery 2, 221-224.
- Chandra, P.S. (2013). Why are neurosurgeons hesitant to use the K word for aneurysm surgery? Indian Journal of Neurosurgery 2, 001-003.
- Chandra, P.S. (2013). Does a partial excision for craniopharyngioma indicate a defeat for the surgeon? Indian Journal of Neurosurgery 2, 113-114.
- Chandra, P.S. (2014). Aspirin for Prevention of Subarachnoid Hemorrhage: The Stage Is Set for a Randomized Controlled Trial Reply. NEUROSURGERY 74, 148-E150.
- Chandra, P.S. (2015). In reply: distraction, compression, and extension reduction of basilar invagination and atlantoaxial dislocation. Neurosurgery 76, E240-E242.
- Chandra, P.S. (2015). In reply: different facets in management of congenital atlantoaxial dislocation and basilar invagination. Neurosurgery 77, E987-E988.
- Chandra, P.S. (2016). Multiple Choice Question on Epilepsy Surgery (Correct Answer is in Bold and Underlined). International Journal of Epilepsy 3, 106-107.
- Chandra, P.S. (2019). Craniovertebral Junction Anomalies: Changing Paradigms, Shifting Perceptions: Where Are We and Where Are We Going? Neurospine 16, 209.
- Chandra, P.S. (2019). We Stand on the Shoulders of Our Teachers… So that We Can See Further…. Neurology India 67, 964.
- Chandra, P.S. (2019). Pediatric Epilepsy Surgery: Preoperative Assessment and Surgical Treatment. Neurology India 67, 1399.
- Chandra, P.S. (2019). The Unbearable Suffering Followed by Ineffable Relief of a Good Doctor: Tuberculosis as a Malady, Still Rules the Roost. Neurology India 67, 1405.
- Chandra, P.S. (2019). The Cover Page Comment. In. (WOLTERS KLUWER MEDKNOW PUBLICATIONS WOLTERS KLUWER INDIA PVT LTD, A-202, 2ND….
- Chandra, P.S. (2020). Are there any indications of transoral odontoidectomy today? Neurosurgical Focus: Video 3, V7.
- Chandra, P.S. (2020). The Need for Uniform Residency Training Programs and the challenges during COVID Pandemic for India. Neurology India 68, 1279.
- Chandra, P.S. (2021). Starting Elective Neurosurgeries: Recovering From COVID Pandemic. Neurology India 69, 2.
- Chandra, P.S. (2021). Basal Cisternostomy: Hype or Hope? Neurology India 69, 243.
- Chandra, P.S., and Agarwal, M. (2020). A case of severe basilar invagination and AAD, corrected using the technique of DCER—distraction, compression, extension, reduction (with spacer+ universal reducer). Neurosurgical Focus: Video 3, V9.
- Chandra, P.S., Ansari, A., Chauhan, A., Kumar, A., Garg, A., Sarkar, C., Bal, C., and Tripathi, M. (2012). Surgery for encephalomalacias presenting with intractable epilepsy. Indian Journal of Neurosurgery 1, 033-037.
- Chandra, P.S., Bajaj, J., Singh, P.K., Garg, K., and Agarwal, D. (2019). Basilar invagination and atlantoaxial dislocation: reduction, deformity correction and realignment using the DCER (distraction, compression, extension, and reduction) technique with customized instrumentation and implants. Neurospine 16, 231.
- Chandra, P.S., Bajaj, J., Subianto, H., and Tripathi, M. (2019). 23 Endoscopic-Assisted Hemispherotomy. Operative Techniques in Epilepsy Surgery.
- Chandra, P.S., Brockmeyer, D., Mendel, E., and Patkar, S.V. (2020). Introduction: Intraoperative manipulation, reduction, realignment, and deformity reduction in patients with atlantoaxial dislocation and basilar invagination. Neurosurgical Focus: Video 3, V1.
- Chandra, P.S., Doddamani, R., Girishan, S., Samala, R., Agrawal, M., Garg, A., Ramanujam, B., Tripathi, M., Bal, C., and Nehra, A. (2021). Robotic thermocoagulative hemispherotomy: concept, feasibility, outcomes, and safety of a new “bloodless” technique. Journal of Neurosurgery: Pediatrics 1, 1-12.
- Chandra, P.S., Garg, A., Sarkar, C., Kurwale, N., Chibber, S.S., Tripathi, M., Bal, C., and Tripathi, M. (2016). Endoscopic assisted inter hemispheric trans-callosal hemispherotomy: Preliminary description of a novel technique. International Journal of Epilepsy 3, A15.
- Chandra, P.S., Garg, A., Sarkar, C., Kurwale, N., Chibber, S.S., Tripathi, M., Bal, C., and Tripathi, M. (2016). Endoscopic assisted (through a mini craniotomy) corpus callostomy combined with anterior, hippocampal, and posterior commissurotomy in Lennox Gastaut syndrome: A pilot study to establish its safety and efficacy. International Journal of Epilepsy 3, A16.
- Chandra, P.S., Ghonia, R., Singh, S., and Garg, K. (2021). Anomalous Vertebral Artery During Cranio Vertebral Junction Surgery Using DCER (Distraction, Compression, Extension, and Reduction): Approach. and Its Repair. Neurology India 69, 315.
- Chandra, P.S., and Goyal, N. (2015). In reply: the severity of basilar invagination and atlantoaxial dislocation correlates with sagittal joint inclination, coronal joint inclination, and craniocervical tilt: a description of new indices for the craniovertebral junction. Neurosurgery 76, E235-E239.
- Chandra, P.S., Goyal, N., Chauhan, A., Ansari, A., Sharma, B.S., and Garg, A. (2014). The severity of basilar invagination and atlantoaxial dislocation correlates with sagittal joint inclination, coronal joint inclination, and craniocervical tilt: a description of new indexes for the craniovertebral junction. Operative Neurosurgery 10, 621-630.
- Chandra, P.S., Gulati, S., Kalra, V., Garg, A., Mishra, N.K., Bal, C., Sarkar, C., and Tripathi, M. (2011). Fourth ventricular hamartoma presenting with status epilepticus treated with emergency surgery in an infant. Pediatric neurosurgery 47, 217-222.
- Chandra, P.S., Gupta, A., Mishra, N.K., and Mehta, V.S. (2005). Association of craniovertebral and upper cervical anomalies with dermoid and epidermoid cysts: report of four cases. Neurosurgery 56, E1155-E1155.
- CHANDRA, P.S., JAIN, S., and TRIPATHI, M. (2008). Electrocorticography for epilepsy surgery—‘Spike chasing’is worthwhile. Progress in Clinical Neurosciences 23, 229.
- Chandra, P.S., Jaiswal, A., and Mahapatra, A. (2002). Bifrontal epidural haematomas following surgery for occipital falcine meningioma: an unusual complication of surgery in the prone position. Journal of clinical neuroscience 9, 582-584.
- Chandra, P.S., Kamal, R., and Mahapatra, A. (1999). An unusual case of dorsally situated bony spur in a lumbar split cord malformation. Pediatric neurosurgery 31, 49-52.
- Chandra, P.S., and Kaur, K.D. (2019). Development of a unique retractor for performing endoscopic pituitary surgery-EASYTRAC. Neurology India 67, 1509.
- Chandra, P.S., Kumar, A., Chauhan, A., Ansari, A., Mishra, N.K., and Sharma, B.S. (2013). Distraction, compression, and extension reduction of basilar invagination and atlantoaxial dislocation. Neurosurgery 72, 1040-1053.
- Chandra, P.S., Kurwale, N., Garg, A., Dwivedi, R., Malviya, S.V., and Tripathi, M. (2015). Endoscopy-assisted interhemispheric transcallosal hemispherotomy: preliminary description of a novel technique. Neurosurgery 76, 485-495.
- Chandra, P.S., and Mahapatra, A. (2012). li34 Traumatic Basal Ganglia. Textbook of Traumatic Brain Injury, 207.
- Chandra, P.S., and Mahapatra, A. (2012). Prevention of Head Injuries. Textbook of Traumatic Brain Injury, 318.
- Chandra, P.S., and Mahapatra, A. (2012). Traumatic Basal Ganglia Hematomas and Infarcts. Textbook of Traumatic Brain Injury, 207.
- Chandra, P.S., Manjari, T., Chandramouli, B.A., Jayakumar, P., and Shankar, S. (1999). Cavernous-venous malformation of brain stem—report of a case and review of literature. Surgical neurology 52, 280-285.
- Chandra, P.S., Mehta, V., and Agarwal, S. (2004). Head Injuries and Psychiatric Disturbances. Mental Health: An Indian Perspective (1946-2003) Elsevier: New Delhi, 306-312.
- Chandra, P.S., Padma, V.M., Shailesh, G., Chandreshekar, B., Sarkar, C., and Tripathi, M. (2008). Hemispherotomy for intractable epilepsy. Neurology India 56, 127.
- Chandra, P.S., and Pandey, P. (2014). Minimally invasive spine surgery: Adapting to a new technology. Indian Journal of Neurosurgery 3, 001-002.
- Chandra, P.S., Prabhu, M., Goyal, N., Garg, A., Chauhan, A., and Sharma, B.S. (2015). Distraction, compression, extension, and reduction combined with joint remodeling and extra-articular distraction: description of 2 new modifications for its application in basilar invagination and atlantoaxial dislocation: prospective study in 79 cases. Neurosurgery 77, 67-80.
- Chandra, P.S., Salamon, N., Huang, J., Wu, J.Y., Koh, S., Vinters, H.V., and Mathern, G.W. (2006). FDG‐PET/MRI coregistration and diffusion‐tensor imaging distinguish epileptogenic tubers and cortex in patients with tuberous sclerosis complex: a preliminary report. Epilepsia 47, 1543-1549.
- Chandra, P.S., Samala, R., Agrawal, M., Doddamani, R.S., Ramanujam, B., and Tripathi, M. (2020). Vagal Nerve Stimulation for Drug Refractory Epilepsy. Neurology India 68, 325.
- Chandra, P.S., and Sharma, B. MESSAGE FROM SECRETARY GENERAL, AESC.
- Chandra, P.S., and Singh, P. (2017). In reply: distraction, compression, extension, and reduction combined with joint remodeling and extra-articular distraction: description of 2 new modifications for its application in basilar invagination and atlantoaxial dislocation: prospective study in 79 cases. Neurosurgery 80, 231-235.
- Chandra, P.S., and Singh, P. (2018). Reply to the letter to editor regarding the article “Treatment of vertebral body hemangiomas with direct ethanol injection and short segment stabilization”. The Spine Journal 18, 2372-2373.
- Chandra, P.S., Singh, P.K., Goyal, V., Chauhan, A.K., Thakkur, N., and Tripathi, M. (2013). Early versus delayed endoscopic surgery for carpal tunnel syndrome: prospective randomized study. World neurosurgery 79, 767-772.
- Chandra, P.S., Subianto, H., Bajaj, J., Girishan, S., Doddamani, R., Ramanujam, B., Chouhan, M.S., Garg, A., Tripathi, M., and Bal, C.S. (2018). Endoscope-assisted (with robotic guidance and using a hybrid technique) interhemispheric transcallosal hemispherotomy: a comparative study with open hemispherotomy to evaluate efficacy, complications, and outcome. Journal of Neurosurgery: Pediatrics 23, 187-197.
- Chandra, P.S., Tej, M., Sawarkar, D., Agarwal, M., and Doddamani, R.S. (2020). Fronto-Orbital Variant of Supraorbital Keyhole Approach for Clipping Ruptured Anterior Circulation Aneurysms (f-Sokha). Neurology India 68, 1019.
- Chandra, P.S., and Tripathi, M. (2010). Epilepsy surgery: recommendations for India. Annals of Indian Academy of Neurology 13, 87.
- Chandra, P.S., and Tripathi, M. (2016). Letter to the editor: Endoscope-assisted hemispherotomy and corpus callostomy. Journal of Neurosurgery: Pediatrics 18, 141-144.
- Chandra, P.S., and Tripathi, M. (2019). Letter to the Editor. Endoscope-assisted hemispherotomy. Journal of Neurosurgery: Pediatrics 25, 326-327.
- Chandra, P.S., and Tripathi, M. (2019). Endoscopic hemispherotomy Response. JOURNAL OF NEUROSURGERY-PEDIATRICS 24, 734-734.
- Chandra, S. Available online at www. sciencedirect. com.
- Chandra, S., Bal, C., Jain, S., Joshua, S., Gaikwad, S., and Garg, A. (2013). Intra-operative co-registration of MRI, PET and electrocorticographic data for neocortical lesional epilepsies may improve the localization of the epileptogenic focus: a pilot study. World Neurosurg 82, 110-117.
- Chandra, S., Chaudhary, N., Deepak, K., Padma, V., and Tripathi, M. (2009). EFFECT OF VAGAL NERVE STIMULATION (VNS) ON CARDIOVASCULAR AUTONOMIC FUNCTIONS IN REFRACTORY EPILEPTIC PATIENTS: E755. Epilepsia 50.
- CHANDRA, S., CHEN, E., COUSIN, T., and ODA, D. (2017). INTRAOSSEOUS HEMANGIOMA OF MANDIBLE AND MAXILLA: A RARE PRESENTATION OF SIX CASES. Oral surgery, oral medicine, oral pathology and oral radiology 124, e224.
- Chandra, S., Dagar, A., Chaudhary, K., Chauhan, A., Bal, C., Garg, A., Sarkar, C., Gaikwad, S., Diwedi, R., and Madakasira, P. (2011). TO ASSESS THE CHILDREN OPERATED FOR DRUG RESISTANT EPILEPSY FROM A LARGE TERTIARY CARE CENTER IN INDIA: p609. Epilepsia 52.
- Chandra, S., Garg, K., Gupta, V., Goel, M., Diwedi, R., Chaudhary, K., Padma, V., Garg, A., Singh, M., and Bal, C. (2013). LONG TERM OUTCOME IN PERSONS WITH DRUG REFRACTORY EPILEPSY AFTER RESECTION IN UNILATERAL MESIAL TEMPORAL SCLEROSIS: P590. Epilepsia 54.
- Chandra, S., Goyal, M., Mishra, N., and Gaikwad, S. (2000). Invasive aspergillosis presenting as a cavernous sinus mass in immuno competent individuals; report of 3 cases. Neuroradiology 42, 108-111.
- ]Chandra, S., Kumar, S., and Singh, A. (1998). Management of Cercospora leaf spot of groundnut (Arachis hypogaea L.) with a single fungicidal spray. International Journal of Pest Management 44, 135-137.
- ]Chandra, S., Kumar, V., and Kumar, A. (2020). A correlative study to predict esophageal varices grading with aspartate aminotransferase to platelet ratio index (apri) in patients of liver cirrhosis. The Journal of the Association of Physicians of India 68, 90.
- Chandra, S., Mathern, G., Wu, J., Koh, S., Sankar, R., and Salamon, N. (2005). LARGER FDG-PET HYPOMETABOLISM ON MRI/PET FUSION STUDIES DETECTS THE EPILEPTIC FOCUS NON-INVASIVELY IN TUBEROUS SCLEROSIS COMPLEX PATIENTS: 2.460. Epilepsia 46.
- Chandra, S., Mukherjee, S., and Sethi, N. (1972). Effect of argemone oil feeding on blood biochemistry and tissue changes in albino rats. Indian journal of medical sciences 26, 308-312.
- Chandra, S., Padma, V., Singh, M., Srivastava, A., Gaikwad, S., Gupta, A., Sarkar, C., Bal, C., and Tripathi, M. (2007). EPILEPSY SURGERY FOR PAEDIATRIC PATIENTS: A REVIEW FROM A LARGE TERTIARY CENTRE (AIIMS, NEW DELHI) p388. Epilepsia 48.
- Chandra, S., Sanyal, S., Gupta, S., Singh, V., Bhatia, M., Gaikwad, S., Tripathi, M., and Mehta, V. (2003). Neuropsychological Assessment and Outcome Following Surgery for Intractable Epilepsy using Specially Developed Battery for Indian Patients. Epilepsia 44.
- Chandra, S., Singh, A., Khan, S., and Singh, V. (2008). Cognitive and behavior problems in patient's taking antiepileptic drugs. The International Journal of Neuropsychopharmacology 11, 194.
- Chandra, S., and Tripathi, M. (2018). Endoscopic Assisted Hemispherotomy: A Comparative Study with Open Hemispherotomy to Evaluate Efficacy, Complications and Outcome. In EPILEPSIA. (WILEY 111 RIVER ST, HOBOKEN 07030-5774, NJ USA), pp S44-S44.
- Chandra, S., Tripathi, M., Mukherjee, S., Deepak, K., and Madakasira, P. (2004). COMPARISON OF AUTONOMIC FUNCTIONS BETWEEN PATIENTS OF WELL-CONTROLLED AND INTRACTABLE EPILEPSY: 1.049. Epilepsia 45.
- Chandra, S.P. Electrocorticography In Epilepsy Surgery: Its Role And Controversies.
- Chandra, S.P. (2015). In Reply to the Letter to the Editor regarding Analysis of Changing Paradigms of Management in 179 Patients with Spinal Tuberculosis During a 12-Year Period and Proposal of a New Management Algorithm. World neurosurgery 84, 2072-2073.
- Chandra, S.P. (2018). Techniques for reduction of basilar invagination and atlanto axial dislocation and surgical instruments thereof. In. (US Patent 9,924,977.
- Chandra, S.P., Bajaj, J., Ghonia, R., and Doddamani, R. (2020). Video Section-Operative Nuances: Step by Step–Single Stage Clipping of Ruptured Middle Cerebral Artery and Unruptured Basilar Top Aneurysm. Neurology India 68, 800.
- Chandra, S.P., Bal, C., Giakwad, S., Padma, V., Srivasatava, A., and Tripathi, M. (2008). S2-3 Epilepsy surgery in India Experience of 473 cases over 10 years from a large tertiary center in India (Drug resistance and epilepsy surgery in Asia, The 42^< nd> Congress of the Japan Epilepsy Society). てんかん研究 26, 250-251.
- Chandra, S.P., Bal, C., Jain, S., Joshua, S.P., Gaikwad, S., Garg, A., Ansari, A., Nehra, A., Sarkar, C., and Tripathi, M. Peer-Review Reports. surgery 31, 34.
- Chandra, S.P., Bal, C., Jain, S., Joshua, S.P., Gaikwad, S., Garg, A., Ansari, A., Nehra, A., Sarkar, C., and Tripathi, M. (2014). Intraoperative coregistration of magnetic resonance imaging, positron emission tomography, and electrocorticographic data for neocortical lesional epilepsies may improve the localization of the epileptogenic focus: a pilot study. World neurosurgery 82, 110-117.
- Chandra, S.P., and Kumar, A. (2012). Clipping of a re-grown basilar bifurcation aneurysm following coiling: An extreme surgical challenge. Neurology India 60, 676.
- Chandra, S.P., Kurwale, N.S., Chibber, S.S., Banerji, J., Dwivedi, R., Garg, A., Bal, C., Tripathi, M., Sarkar, C., and Tripathi, M. (2016). Endoscopic-assisted (through a mini craniotomy) corpus callosotomy combined with anterior, hippocampal, and posterior commissurotomy in Lennox-Gastaut syndrome: a pilot study to establish its safety and efficacy. Neurosurgery 78, 743-751.
- Chandra, S.P., Ramdurg, S.R., Kurwale, N., Chauhan, A., Ansari, A., Garg, A., Sarkar, C., and Sharma, B.S. (2014). Extended costotransversectomy to achieve circumferential fusion for pathologies causing thoracic instability. The Spine Journal 14, 2094-2101.
- Chandra, S.P., Singh, A., Goyal, N., Laythalling, R.K., Singh, M., Kale, S.S., Sharma, M.S., Suri, A., Singh, P., and Garg, A. (2013). Analysis of changing paradigms of management in 179 patients with spinal tuberculosis over a 12-year period and proposal of a new management algorithm. World neurosurgery 80, 190-203.
- Chandra, S.P., Singh, P., Kumar, R., Agarwal, D., Tandon, V., Kale, S.S., and Sarkar, C. (2019). Long-term outcome of treatment of vertebral body hemangiomas with direct ethanol injection and short-segment stabilization. The Spine Journal 19, 131-143.
- Chandra, S.P., and Tripathi, M. (2015). Endoscopic epilepsy surgery: Emergence of a new procedure. Neurology India 63, 571.
- Chaudhari, R.M., Dash, D., Ramanujam, B., Rana, M.K., Appukuttan, R., Sharma, A., Kunwar, Y., Tejaniya, G., Padma, V., and Chandra, S.P. (2016). Evaluation of Ictal Consciousness in Temporal and Extra Temporal Epilepsy: Observations from a Tertiary Care Hospital in India. Journal of epilepsy research 6, 95.
- Chaudhari, R.M., Ramanujam, B., Appukuttan, R., Sharma, A., Kunwar, Y., Tejaniya, G., Garg, A., Padma, M.V., Tripathi, M., and Bal, C. (2017). Utility of a questionnaire tool (QUARAS) for localizing and lateralizing seizures in the epilepsy monitoring unit (EMU). Clinical neurology and neurosurgery 153, 64-66.
- Chaudhary, K., Kumaran, S., Chandra, S.P., Wadhawan, A.N., and Tripathi, M. Language reorganization in pre-and post-operative drug refractory extra temporal lobe epilepsy patients: An fMRI based study.
- Chaudhary, K., KUMARAN, S.S., Chandra, P.S., and Tripathi, M. Effect of temporal lobe epilepsy on language function revealed by fMRI.
- Chaudhary, K., Kumaran, S.S., Chandra, S.P., Wadhawan, A.N., and Tripathi, M. (2014). Mapping of cognitive functions in chronic intractable epilepsy: Role of fMRI. The Indian journal of radiology & imaging 24, 51.
- Chaudhary, K., Kumaran, S.S., Tripathi, M., and Chandra, S.P. Semantic memory processing in left temporal lobe epilepsy using functional Magnetic Resonance Imaging. Insula 13, 10.
- Chaudhary, K., Kumaran, S.S., Tripathi, M., and Chandra, S.P. Language processing in temporal lobe epilepsy and extra temporal lobe epilepsy using functional MRI.
- Chaudhary, K., Ramanujam, B., Kumaran, S., Chandra, P., Nehra, A., and Tripathi, M. (2017). SEMANTIC VERBAL MEMORY OUTCOME AFTER SURGERY IN DRUG REFRACTORY EPILEPSY: AN FMRI BASED STUDY. In EPILEPSIA. (WILEY 111 RIVER ST, HOBOKEN 07030-5774, NJ USA), pp S122-S123.
- Chaudhary, K., Ramanujam, B., Kumaran, S.S., Chandra, P.S., Wadhawan, A.N., Garg, A., and Tripathi, M. (2017). Does education play a role in language reorganization after surgery in drug refractory temporal lobe epilepsy: An fMRI based study? Epilepsy research 136, 88-96.
- Chaudhary, K., Tripathi, M., Chandra, P.S., Nehra, A., and Kumaran, S.S. (2020). Evaluation of memory in persons with mesial temporal lobe sclerosis: A combined fMRI and VBM study. Journal of Biosciences 45, 1-11.
- Chauhan, A.K., Chandra, P.S., Goyal, N., Chowdhury, M.R., Banerjee, J., Tripathi, M., and Kabra, M. (2020). Weak ligaments and sloping joints: a new hypothesis for development of congenital atlantoaxial dislocation and basilar invagination. Neurospine 17, 843.
- Choudhary, K.S., Doddamani, R.S., Devarajan, L.J., Agrawal, M., Sawarkar, D., Meena, R.K., Varma, S., Kumar, A., Singh, P., and Chandra, P.S. (2020). Feasibility of Double Anterior Odontoid Screw: A CT-Based Morphometric Analysis of the Axis in Adult Indian Population. Neurology India 68, 1361.
- Choudhary, N., Deepak, K.K., Chandra, P.S., Bhatia, S., Sagar, R., Jaryal, A.K., Pandey, R.M., and Tripathi, M. (2017). Comparison of autonomic function before and after surgical intervention in patients with temporal lobe epilepsy. Journal of epilepsy research 7, 89.
- Dagar, A., Chandra, P.S., Chaudhary, K., Avnish, C., Bal, C., Gaikwad, S., Garg, A., Sarkar, C., Srivastava, A., and Padma, M. (2011). Epilepsy surgery in a pediatric population: a retrospective study of 129 children from a tertiary care hospital in a developing country along with assessment of quality of life. Pediatric neurosurgery 47, 186-193.
- Darbari, S., Meena, R.K., Sawarkar, D., Doddamani, R.S., Singh, M., and Chandra, P.S. (2019). Intraventricular Meningioma Presenting as Lateral Posterior Choroidal Artery Stroke. World neurosurgery 125, 364-367.
- Dash, C., Moorthy, S., Garg, K., Singh, P.K., Kumar, A., Gurjar, H., Chandra, P.S., and Kale, S.S. (2019). Management of choroid plexus tumors in infants and young children up to 4 years of age: an institutional experience. World neurosurgery 121, e237-e245.
- Deb, P., Sharma, M., Tripathi, M., Sarat Chandra, P., Gupta, A., and Sarkar, C. (2006). Expression of CD34 as a novel marker for glioneuronal lesions associated with chronic intractable epilepsy. In. (Blackwell Publishing Ltd Oxford, UK.
- Deb, P., Sharma, M.C., Gaikwad, S., Tripathi, M., Chandra, P.S., Jain, S., and Sarkar, C. (2005). Neuropathological spectrum of Rasmussen encephalitis. Neurology India 53, 156.
- Deora, H., Mishra, S., Tripathi, M., Garg, K., Tandon, V., Borkar, S., Varshney, N., Raut, R., Chaurasia, B., and Chandra, P.S. (2020). Adapting neurosurgery practice during the COVID-19 pandemic in the Indian subcontinent. World neurosurgery 142, e396-e406.
- Deora, H., Sadashiva, N., Tripathi, M., Yagnick, N.S., Mohindra, S., Batish, A., Patil, N.R., Aggarwal, A., Jangra, K., and Bhagat, H. (2020). The Aftermath of COVID-19 Lockdown-Why and How Should We Be Ready? Neurology India 68, 774.
- Desai, S., Shukla, G., Goyal, V., Srivastava, A., Srivastava, M.P., Tripathi, M., Singh, M., Shivanand, K., Sagar, R., and Gupta, A. (2014). Changes in psychiatric comorbidity during early postsurgical period in patients operated for medically refractory epilepsy—a MINI-based follow-up study. Epilepsy & Behavior 32, 29-33.
- Dey, S., Dixit, A., Tripathi, M., Chandra, P.S., and Banerjee, J. (2018). Role of Pyridoxal Phosphate in Modulation of Endogenous Kynurenic Acid Synthesis Associated with Hippocampal Sclerosis. International Journal of Epilepsy 5, A0042.
- Dey, S., Dixit, A.B., Tripathi, M., Chandra, P.S., and Banerjee, J. (2016). Endogenous kynurenic acid, a tryptophan metabolite, synthesis is altered in resected brain specimens obtained from patients with mesial temporal lobe epilepsy. International Journal of Epilepsy 3, A40.
- Dey, S., Dixit, A.B., Tripathi, M., Doddamani, R., Sharma, M., Lalwani, S., Chandra, S., and Banerjee, J. (2020). Altered hippocampal kynurenine pathway metabolism contribute to hyperexcitability in mesial temporal lobe epilepsy-hippocampal sclerosis. Authorea Preprints.
- Dikshit, B., Irshad, K., Madan, E., Aggarwal, N., Sarkar, C., Chandra, P., Gupta, D., Chattopadhyay, P., Sinha, S., and Chosdol, K. (2013). FAT1 acts as an upstream regulator of oncogenic and inflammatory pathways, via PDCD4, in glioma cells. Oncogene 32, 3798-3808.
- Dixit, A., Banerjee, J., Srivastava, A., Tripathi, M., Sarkar, C., Kakkar, A., and Chandra, P. (2015). RNA-SEQ ANALYSIS OF HIPPOCAMP AL TISSUES REVEALS NOVEL CANDIDATE GENES FOR DRUG REFRACTORY EPILEPSY IN PATIENTS WITH MTLE-HS: p0148. Epilepsia 56, 44-45.
- Dixit, A.B. (2015). RNA-seq analysis of hippocampal tissues reveals novel candidate genes for drug refractory epilepsy in patients with MTLE-HS.
- Dixit, A.B., Banerjee, J., Ansari, A., Tripathi, M., and Chandra, S.P. (2016). Mutations in GABRG2 receptor gene are not a major factor in the pathogenesis of mesial temporal lobe epilepsy in Indian population. Annals of Indian Academy of Neurology 19, 236.
- Dixit, A.B., Banerjee, J., Chandra, P.S., and Tripathi, M. (2017). Recent advances in epilepsy research in India. Neurology India 65, 83.
- Dixit, A.B., Banerjee, J., Srivastava, A., Tripathi, M., Sarkar, C., Kakkar, A., Jain, M., and Chandra, P.S. (2016). RNA-seq analysis of hippocampal tissues reveals novel candidate genes for drug refractory epilepsy in patients with MTLE-HS. Genomics 107, 178-188.
- Dixit, A.B., Banerjee, J., Tripathi, M., and Chandra, P.S. (2015). Presurgical epileptogenic network analysis: A way to enhance epilepsy surgery outcome. Neurology India 63, 743.
- Dixit, A.B., Banerjee, J., Tripathi, M., Sarkar, C., and Chandra, P.S. (2017). Synaptic roles of cyclin-dependent kinase 5 & its implications in epilepsy. The Indian journal of medical research 145, 179.
- Dixit, A.B., Paul, D., Srivastava, A., Banerjee, J., Tripathi, M., and Chandra, P.S. (2016). Differential modulation of various inflammatory mediators in mesial temporal lobe epilepsy and focal cortical dysplasia patients. International Journal of Epilepsy 3, A6.
- Dixit, A.B., Sharma, D., Srivastava, A., Banerjee, J., Tripathi, M., Prakash, D., and Chandra, P.S. (2017). Upregulation of breast cancer resistance protein and major vault protein in drug resistant epilepsy. Seizure 47, 9-12.
- Dixit, A.B., Sharma, D., Tripathi, M., Srivastava, A., Paul, D., Prakash, D., Sarkar, C., Kumar, K., Banerjee, J., and Chandra, P.S. (2018). Genome-wide DNA methylation and RNAseq analyses identify aberrant signalling pathways in focal cortical dysplasia (FCD) Type II. Scientific reports 8, 1-12.
- Dixit, A.B., Srivastava, A., Sharma, D., Tripathi, M., Paul, D., Lalwani, S., Doddamani, R., Sharma, M., Banerjee, J., and Chandra, P.S. (2020). Integrated genome-wide DNA methylation and RNAseq analysis of hippocampal specimens identifies potential candidate genes and aberrant signalling pathways in patients with hippocampal sclerosis. Neurology India 68, 307.
- Dixit, A.B., Tripathi, M., Chandra, P.S., and Banerjee, J. (2016). Molecular biomarkers in drug-resistant epilepsy: Facts & possibilities. International Journal of Surgery 36, 483-491.
- Doddamani, R.S., Agrawal, M., Samala, R., Ramanujam, B., Chandra, P.S., and Tripathi, M. (2020). Vagal Nerve Stimulation in the Management of Epilepsy-Recent Concepts. Neurology India 68, 259.
- Doddamani, R.S., and Chandra, P.S. (2019). Aneurysmal SAH “A Riddle Wrapped Up in Enigma”. Neurology India 67, 1290.
- Doddamani, R.S., Meena, R., Samala, R., Agrawal, M., Tripathi, M., and Chandra, P.S. (2021). Expanding the Horizons of mTOR Inhibitors for Treating Subependymal Giant Cell Astrocytomas with Obstructive Hydrocephalus. Pediatric Neurosurgery 56, 102-104.
- Doddamani, R.S., Meena, R., Sawarkar, D., Singh, P., Agrawal, D., Singh, M., and Chandra, P.S. (2021). Robot-guided Ventriculoperitoneal Shunt in Slit-like Ventricles. Neurology India 69, 446.
- Doddamani, R.S., Meena, R., Sawarkar, D., Singh, P.K., and Chandra, P.S. (2021). Stereotactic guided ablation for subependymal giant cell astrocytomas: does it change the surgical indications? Child's Nervous System 37, 735-736.
- Doddamani, R.S., Meena, R.K., Sawarkar, D., Aggarwal, D., and Chandra, P.S. (2020). Management Options in Occipital Neuralgia: A. Journal of Peripheral Nerve Surgery Vol 4.
- Doddamani, R.S., Samala, R., Agrawal, M., Verma, R., Kumar, N., and Chandra, P.S. (2020). Robotic Guided Bilateral Anterior Cingulate Radiofrequency Ablation for Obsessive-Compulsive Disorder. Neurology India 68, 333.
- Doddamani, R.S., Sawarkar, D., Meena, R.K., Gurjar, H., Singh, P.K., Singh, M., Chandra, P.S., and Sathyarthee, G. (2019). Remote cerebellar hemorrhage following surgery for supratentorial lesions. World neurosurgery 126, e351-e359.
- Doddamani, R.S., Tripathi, M., Samala, R., Agarwal, M., Ramanujan, B., and Chandra, S.P. (2020). Posterior quadrant disconnection for sub-hemispheric drug refractory epilepsy. Neurology India 68, 270.
- Doddamani, R.S., Tripathi, M., Samala, R., Agrawal, M., Ramanujam, B., Bajaj, J., Girishan, S., Tripathi, M., Bal, C., and Garg, A. (2020). Hypothalamic hamartoma and endocrinopathy: A neurosurgeon's perspective. Neurology India 68, 146.
- Dube, S.K., Mahajan, C., Chouhan, R.S., Dash, H.H., Rath, G.P., Suri, A., Chandra, P., and Mahajan, A. Effect of Intraoperative Brain Protection With Propofol on Postoperative Cognition in Patients Undergoing Temporary Clipping During Intracranial Aneurysm Surgery.
- Dwivedi, R., Ramanujam, B., Chandra, P.S., Sapra, S., Gulati, S., Kalaivani, M., Garg, A., Bal, C.S., Tripathi, M., and Dwivedi, S.N. (2017). Surgery for drug-resistant epilepsy in children. New England Journal of Medicine 377, 1639-1647.
- Elavarasi, A., Chandra, S., Garg, A., Viswanathan, V., Bharti, K., Bal, C.S., Tripathi, M., Sharma, M.C., Pandey, R., and Dash, D. (2018). Magnetoencephalography in Epilepsy surgery: Concordance and Yield (P1. 276). In. (Wolters Kluwer Health, Inc. on behalf of the American Academy of Neurology.
- Fallah, A., Weil, A.G., Lewis, E.C., Ibrahim, G.M., Kola, O., Tseng, C.-H., Zhou, X., Lin, K.-M., Cai, L.-X., and Liu, Q.-Z. (2020). Hemispheric Surgery Outcome Prediction Scale: Development and Validation of a Seizure Freedom Prediction Tool.
- Gaonkar, V.B., Garg, K., Agrawal, D., Chandra, P.S., and Kale, S.S. (2020). Risk factors for progression of conservatively managed acute traumatic subdural hematoma: A systematic review and meta-analysis. World Neurosurgery.
- Garg, A., Chugh, M., Gaikwad, S.B., Chandra, S.P., Gupta, V., Mishra, N.K., and Sharma, M.C. (2004). Juvenile pilocytic astrocytoma presenting with subarachnoid hemorrhage: case report and review of the literature. Journal of Neurosurgery: Pediatrics 100, 525-529.
- Garg, A., Suri, A., Chandra, P., Kumar, R., Sharma, B., and Mahapatra, A. (2009). Endoscopic Third Ventriculostomy. Pediatric neurosurgery 45, 1-5.
- Garg, K., Chandra, P.S., Singh, P.K., and Sharma, B.S. (2013). Giant craniopharyngioma: can it grow bigger than this? Pediatric neurosurgery 49, 124-125.
- Garg, K., Deora, H., Mishra, S., Tripathi, M., Sadashiva, N., Chandra, P.S., and Kale, S.S. (2019). How is neurosurgical residency in India? Results of an anonymized national survey of residents. Neurology India 67, 777.
- Garg, K., Deora, H., Mishra, S., Tripathi, M., Sadashiva, N., Chandra, S.P., and Kale, S.S. (2020). Quality of Neurosurgery Training in India when Compared to UK-Are We There Yet? Neurology India 68, 950.
- Garg, K., Gurjar, H., Singh, P., Satyarthee, G., Singh, M., Chandra, P., and Sharma, B. (2013). Spontaneous rupture of hydrocephalic head. Neurology India 61, 556.
- Garg, K., Gurjar, H.K., Chandra, P.S., and Sharma, B.S. (2014). Suprasellar tuberculoma. British journal of neurosurgery 28, 562-563.
- Garg, K., Gurjar, H.K., Chandra, P.S., and Sharma, B.S. (2014). Pentapathology in Neurofibromatosis 1. The Indian Journal of Pediatrics 81, 980-981.
- Garg, K., Satyarthee, G.D., Dash, C., Singh, P.K., Chandra, P.S., and Sharma, B.S. (2014). Hyperplasia of Cervical Spinous Process Presenting as Subcutaneous Mass. The Indian Journal of Pediatrics 81, 1128-1130.
- Garg, K., Singh, P., Singla, R., Aggarwal, A., Borle, A., Singh, M., Chandra, P., Kale, S., and Mahapatra, A. (2020). Reply to letter-Role of Decompressive Craniectomy in Traumatic Brain Injury-A Meta-analysis of Randomized Controlled Trials. Neurology India 68, 1243-1243.
- Garg, K., Singh, P., Singla, R., Chandra, P., Singh, M., Satyarthhe, G., Gurjar, H., and Sharma, B. (2013). Armored brain-massive bilateral calcified chronic subdural hematoma in a patient with ventriculoperotoneal shunt. Neurology India 61, 548.
- Garg, K., Singh, P.K., Sharma, B.S., Chandra, P.S., Suri, A., Singh, M., Kumar, R., Kale, S.S., Mishra, N.K., and Gaikwad, S.K. (2014). Pediatric intracranial aneurysms—our experience and review of literature. Child's Nervous System 30, 873-883.
- Garg, K., Singh, P.K., Singh, M., Chandra, P.S., and Sharma, B.S. (2013). Long segment spinal epidural extramedullary hematopoiesis. Surgical neurology international 4.
- Garg, K., Singh, P.M., Singla, R., Aggarwal, A., Borle, A., Singh, M., Chandra, P.S., Kale, S.S., and Mahapatra, A.K. (2019). Role of decompressive craniectomy in traumatic brain injury–A meta-analysis of randomized controlled trials. Neurology India 67, 1225.
- Garg, K., Sinha, S., Kale, S., Chandra, P., Suri, A., Singh, M., Kumar, R., Sharma, M., Pandey, R., and Sharma, B. (2013). Role of simvastatin in prevention of vasospasm and improving functional outcome after aneurysmal sub-arachnoid hemorrhage: a prospective, randomized, double-blind, placebo-controlled pilot trial. British journal of neurosurgery 27, 181-186.
- Garg, K., Tandon, V., Sharma, S., Suri, A., Chandra, P.S., Kumar, R., Mahapatra, A.K., and Sharma, B.S. (2015). Quadrigeminal cistern arachnoid cyst: a series of 18 patients and a review of literature. British journal of neurosurgery 29, 70-76.
- Garg, K., Vij, V., Garg, A., Singh, M., and Chandra, P.S. (2021). “Malignant” Craniospinal Neurocysticercosis: A Rare Case. World Neurosurgery 146, 95-102.
- Garg, M., Kumar, A., Singh, P.K., Agrawal, D., Satyarthee, G.D., Gupta, D., Gurjar, H.K., Mishra, S., Chandra, P.S., and Kale, S.S. (2019). Single-Stage Transpedicular Approach for Circumferential Arthrodesis in Traumatic Lumbar Vertebral Body Burst Fractures. Indian Journal of Neurotrauma 16, 14-20.
- Garg, M., Kumar, A., Singh, P.K., Mahalangikar, R., Satyarthee, G.D., Agrawal, D., Gupta, D., Gurjar, H.K., Mishra, S., and Chandra, P.S. (2021). Transpedicular Approach for Corpectomy and Circumferential Arthrodesis in Traumatic Lumbar Vertebral Body Burst Fractures: A Retrospective Analysis of Outcome in 35 Patients. Neurology India 69, 399.
- Garg, M., Shambanduram, S., Singh, P.K., Sebastian, L.J.D., Sawarkar, D.P., Kumar, A., Gaikwad, S., Chandra, P., and Kale, S.S. (2018). Management of pediatric posterior circulation aneurysms—12-year single-institution experience. World neurosurgery 116, e624-e633.
- Gaur, R., and Chandra, P. (1982). Studies on Weeds of Eleusine Fields in Relation to Soil Nature. Indian Forester 108, 708-711.
- Girishan, S., Tripathi, M., Garg, A., Doddamani, R., Bajaj, J., Ramanujam, B., and Chandra, P.S. (2019). Enhancing outcomes of endoscopic vertical approach hemispherotomy: understanding the role of “temporal stem” residual connections causing recurrence of seizures. Journal of Neurosurgery: Pediatrics 25, 159-167.
- Godil, S.S., Parker, S.L., Zuckerman, S.L., Mendenhall, S., Cheng, J.S., McGirt, M., McGirt, M., Asher, A.L., Speroff, T., and Glassman, S.D. (2013). 271. Predictors of Loss of Kyphotic Deformity Correction and Scoliosis after Anterolateral Vertebrectomy and Spinal Fusion for Thoracolumbar Burst Fractures. Neurosurgical Focus 34, A1-A29.
- Goel, R.K., Ahmad, F.U., Vellimana, A.K., Suri, A., Chandra, P.S., Kumar, R., Sharma, B.S., and Mahapatra, A.K. (2008). Endoscopic management of intraventricular neurocysticercosis. Journal of Clinical Neuroscience 15, 1096-1101.
- Goyal, N., Gurjar, H., Sharma, B.S., Tripathi, M., and Chandra, P.S. (2014). GAPO syndrome with pansutural craniosynostosis leading to intracranial hypertension. Case Reports 2014, bcr2013201727.
- Goyal, N., Kakkar, A., Singh, P.K., Sharma, M.C., Chandra, P.S., Mahapatra, A.K., and Sharma, B.S. (2013). Intracranial teratomas in children: a clinicopathological study. Child's Nervous System 29, 2035-2042.
- Guha, S., Sethi, R., Ray, S., Bahl, V.K., Shanmugasundaram, S., Kerkar, P., Ramakrishnan, S., Yadav, R., Chaudhary, G., and Kapoor, A. (2017). Cardiological Society of India: position statement for the management of ST elevation myocardial infarction in India. Indian heart journal 69, S63.
- Gupta, D.K., Chandra, P., Ojha, B., Sharma, B., Mahapatra, A., and Mehta, V. (2007). Awake craniotomy versus surgery under general anesthesia for resection of intrinsic lesions of eloquent cortex—a prospective randomised study. Clinical neurology and neurosurgery 109, 335-343.
- Gupta, P., Muthukumar, N., Rajshekhar, V., Tripathi, M., Thomas, S., Gupta, S.K., Lal, V., Pal, P., Abraham, M., and Behari, S. (2020). Neurosurgery and neurology practices during the novel COVID-19 pandemic: A consensus statement from India. Neurology India 68, 246.
- Gupta, S., Kumar, S., Singh, R., and Chandra, S. (2005). Identification of a single dominant gene for resistance to Mungbean Yellow Mosaic Virus in blackgram (Vigna mungo (L.) Hepper). SABRAO Journal of Breeding and Genetics 37, 85-89.
- Gupta, V., Garg, A., Chandra, S., Sharma, M., Gaikwad, S., Gulati, S., and Mishra, N. (2003). Cerebellar epilepsy: a case report of a cerebellar gangliomatous hamartoma. Rivista di Neuroradiologia 16, 784-787.
- Gurjar, H., Dwarakanath, S., Sharma, B.S., and Chandra, S. (2008). Cerebellar hemorrhage following endoscopic third ventricular colloid cyst decompression. Neurology India 56, 218.
- Gurjar, H.K., Sarkari, A., and Chandra, P.S. (2012). Surgical management of giant multilevel aneurysmal bone cyst of cervical spine in a 10-year-old boy: case report with review of literature. Evidence-based spine-care journal 3, 55.
- Happe, C., Deacon, D., Erbe, R., Tenerelli, K., Tran, V., Adler, E., Chi, N., Engler, A., Kumar, A., and Thomas, S. (2016). 2016 TERMIS-Americas Conference and Exhibition San Diego, CA December 11–14, 2016. Tissue Engineering Part A 22, S-1-S-156.
- Irshad, K., Mohapatra, S.K., Srivastava, C., Garg, H., Mishra, S., Dikshit, B., Sarkar, C., Gupta, D., Chandra, P.S., and Chattopadhyay, P. (2015). A combined gene signature of hypoxia and notch pathway in human glioblastoma and its prognostic relevance. PloS one 10, e0118201.
- Jackman, C., Heo, S., Bursac, N., Walker, B., Yu, C., Sani, E.S., Kimball, W., Annabi, N., Sapru, S., and Naskar, D. (2017). 2017 TERMIS-Americas Conference & Exhibition Charlotte, NC December 3–6, 2017. Tissue Engineering Part A 23, S-1-S-159.
- JAIN, S., LOPEZ-PERMOUTH, S., TURNWALD, G., CHANDRA, S., KUMAR, V., GUPTA, S.K., MADAN, S., TEWARI, U., and VIRSIK, G. (1995). Series A—Pure Mathematics and Statistics Volume 58 Part3 JUNE 1995.
- Jaiswal, A., and Chandra, P. (2001). Cerebellopontine angle meningioma with acquired chiari and syringomyelia: neuroimage. Neurology India 49, 323.
- Jaiswal, A., Chandra, P., Kamal, R., Sharma, M., and Mahapatra, A. (2000). Cerebellar medulloblastoma in a 65 year old Indian male. Neurology India 48, 178.
- Jaiswal, A.K., Tripathi, M., Chandra, P.S., and Sharma, M. (2000). An unusual case of primary lymphoma of the skull base extending from cerebellopontine angle to cavernous sinus and orbit: A case report. Journal of neurosurgical sciences 44, 145.
- Jayakumar, P., Chandra, P., and Satish, C.P. (1997). Cerebral parenchymal calcification in a child with vein of galen malformation: role of medullary veins. Neurology India 45, 174-176.
- Jayaswal, A., Bhan, S., Dave, P., and Chandra, P. (1985). Modified Phemister grafting in potentially infected non-union of tibial shaft fractures. International surgery 70, 67-70.
- Joaquim, A.F., Tedeschi, H., and Chandra, P.S. (2018). Controversies in the surgical management of congenital craniocervical junction disorders–A critical review. Neurology India 66, 1003.
- Kakkar, A., Majumdar, A., Kumar, A., Tripathi, M., Pathak, P., Sharma, M.C., Suri, V., Tandon, V., Chandra, S.P., and Sarkar, C. (2016). Alterations in BRAF gene, and enhanced mTOR and MAPK signaling in dysembryoplastic neuroepithelial tumors (DNTs). Epilepsy research 127, 141-151.
- Kakkar, A., Majumdar, A., Pathak, P., Kumar, A., Kumari, K., Tripathi, M., Sharma, M.C., Suri, V., Tandon, V., and Chandra, S.P. (2017). BRAF gene alterations and enhanced mammalian target of rapamycin signaling in gangliogliomas. Neurology India 65, 1076.
- Kakkar, A., Majumdar, A., Sharma, M., Suri, V., Tripathi, M., Chandra, S., and Sarkar, C. (2015). PTPS-13STUDY OF CLINICOPATHOLOGICAL CHARACTERISTICS, BRAF V600E MUTATION, AND MTOR SIGNALING PATHWAY ACTIVATION IN DYSEMBRYOPLASTIC NEUROEPITHELIAL TUMORS (DNET). Neuro-oncology 17, v181.
- Kakkar, A., Sharma, M.C., Suri, V., Kaushal, S., Chandra, S.P., Garg, A., and Sarkar, C. (2014). Angiocentric Glioma: A treatable cause of epilepsy: Report of a rare case. Neurology India 62, 677.
- Kakkar, A., Sharma, M.C., Suri, V., Kaushal, S., Chandra, S.P., Garg, A., and Sarkar, C. (2014). Yolk sac tumor of the temporal bone: An unusual presentation as hydrocephalus. Neurology India 62.
- Kale, S., Ailawadhi, P., Yerramneni, V.K., Chandra, P., Kumar, R., Sharma, B., and Mahapatra, A. (2011). Pediatric bony craniovertebral junction abnormalities: Institutional experience of 10 years. Journal of pediatric neurosciences 6, S91.
- Kale, S.S., Chandra, S.P., Suri, A.K., and Mehta, V.S. (2004). 779 One-stage Surgery (Anterior and Posterior) for Craniovertebral Junction Anomalies: Lessons Learned from 632 Cases. Neurosurgery 55, 479.
- Kasliwal, M.K., Chandra, P.S., and Sharma, B.S. (2007). Images in neuro oncology: primary extraaxial cerebellopontine angle ependymoma. Journal of neuro-oncology 83, 31-32.
- Katiyar, V., Garg, K., Doddamani, R., Singh, P.K., Singh, M., and Chandra, P.S. (2020). Spontaneous external rupture of hydrocephalus after fontanelle closure: a case report and review of literature. Child's Nervous System, 1-5.
- Katiyar, V., Sharma, R., Tandon, V., Goda, R., Ganeshkumar, A., Suri, A., Chandra, P.S., and Kale, S.S. (2020). Impact of frailty on surgery for glioblastoma: a critical evaluation of patient outcomes and caregivers’ perceptions in a developing country. Neurosurgical Focus 49, E14.
- Kaur, K., Agrawal, M., Yadav, M., Chandra, P.S., Samala, R., Doddamani, R., Ramanujam, B., Singh, G., and Tripathi, M. (2020). On-scalp Magnetoencephalography: A long but promising road ahead? Clinical Neurophysiology.
- Kaur, K., Chandra, P.S., Samala, R., Agrawal, M., Doddamani, R., Ramanujam, B., Singh, G., and Tripathi, M. (2020). Bridging the gap between analytical methods and their clinical interpretation. Epilepsia 61, 2609-2610.
- Kaur, K., Garg, A., Tripathi, M., Chandra, S.P., Singh, G., Viswanathan, V., Bharti, K., Singh, V., Ramanujam, B., and Bal, C.S. (2021). Comparative contribution of magnetoencephalography (MEG) and single-photon emission computed tomography (SPECT) in pre-operative localization for epilepsy surgery: A prospective blinded study. Seizure 86, 181-188.
- Khan, D., Raj, S., Sagar, S., Tripathi, M., Tripathi, M., Doddamani, R., Garg, A., Chandra, P., Sarkar, C., and Damle, N. (2020). Epileptogenic zone localization on SISCOS in drug refractory epilepsy. In EUROPEAN JOURNAL OF NUCLEAR MEDICINE AND MOLECULAR IMAGING. (SPRINGER ONE NEW YORK PLAZA, SUITE 4600, NEW YORK, NY, UNITED STATES), pp S497-S497.
- Khan, D., ST, A.R., TRIPATHI, M., Garg, A., Tripathi, M., Bhargavi, R., Chandra, P.S., Doddamani, R., Kumar, A., and Bal, C. (2020). Clinical value of FDG-PET and MRI coregistration in Focal Cortical dysplasia.
- Khullar, S., Chandra, P.S., Doddamani, R.S., Kapil, A., and Dhawan, B. (2016). Chronic osteomyelitis of skull due to Pseudomonas aeruginosa: A delayed uncommon complication following craniotomy. Journal of clinical and diagnostic research: JCDR 10, DL01.
- Koyalmantham, V., Garg, K., Sardana, H., Singh, M., and Chandra, P.S. (2017). Holmes’ tremor secondary to a posterior third ventricular germinoma: a rare case report. Child's Nervous System 33, 885-887.
- Koyalmantham, V., Kale, S.S., Devarajan, L.J., Phalak, M., Chandra, P.S., Suri, A., Kumar, R., and Tandon, V. (2020). Patient Outcomes Following Obliteration of Spinal Dural Arteriovenous Fistula and the Role of Indocyanine Green Angiography Videoangiography (ICG‑VA) During Surgery. Neurology India 68, 118.
- Kumar, A., Chandra, P., Bisht, A., Garg, A., Mahapatra, A.K., and Sharma, M. (2011). Successful surgical excision of a nondysraphic holodorsal intramedullary lipoma in a 14-month-old child. Pediatric neurosurgery 47, 272-274.
- Kumar, A., Chandra, P., and Kale, S. (2020). Parietal transventricular approach for medial temporal glioma: A technical report. Surgical neurology international 11.
- Kumar, A., Chandra, P., Mankotia, D.S., Tripathi, M., Garg, A., and Mahapatra, A.K. (2012). Squamosal type superficial middle cerebral vein: a rare venous drainage pattern. Neurology India 60, 546.
- Kumar, A., Chandra, P.S., Sharma, B.S., Garg, A., Rath, G.K., Bithal, P.K., and Tripathi, M. (2014). The role of neuronavigation-guided functional MRI and diffusion tensor tractography along with cortical stimulation in patients with eloquent cortex lesions. British journal of neurosurgery 28, 226-233.
- Kumar, A., Sharma, M.S., Sharma, B.S., Bhatia, R., Singh, M., Garg, A., Kumar, R., Suri, A., Chandra, P.S., and Kale, S.S. (2013). Outcome after decompressive craniectomy in patients with dominant middle cerebral artery infarction: A preliminary report. Annals of Indian Academy of Neurology 16, 509.
- Kumar, A., Shete, V., Singh, M., Satyarthee, G.D., Agrawal, D., Singh, P.K., Sharma, M.C., Chandra, P.S., Laythalling, R.K., and Suri, A. (2019). Intracranial Meningeal Hemangiopericytomas: An Analysis of Factors Affecting Outcome in 39 Cases Managed with Multimodality Treatment. Neurology India 67, 1266.
- Kumar, A., Singh, M., Agrawal, D., Singh, P., Chandra, P., and Kale, S. (2018). Intracranial Meningeal Hemangiopericytomas: An Analysis of Factors Affecting Outcome from Multimodality Treatment of 39 Cases. Journal of Neurological Surgery Part A: Central European Neurosurgery 79, P01.
- Kumar, A., Singh, M., Sharma, M.C., Chandra, P.S., Sharma, B.S., and Mahapatra, A.K. (2017). Giant bicompartmental cystic tentorial schwannoma mimicking a meningioma. World neurosurgery 105, 1038. e1017-1038. e1022.
- Kumar, A., Varshney, G., Singh, P.K., Agrawal, D., Satyarthee, G.D., Chandra, P.S., Kale, S.S., and Mahapatra, A.K. (2018). Traumatic atlantoaxial spondyloptosis associated with displaced odontoid fracture: complete reduction via posterior approach using “joint remodeling” technique. World neurosurgery 110, 609-613.
- Kumar, K., Banerjee, J., Tripathi, M., Chandra, P.S., and Dixit, A.B. (2019). Epigenetic Regulation of mTOR Pathway in Malformations of Cortical Development. Neurology India 67, 1472.
- KUMAR, M.S. (2015). CLIENT.
- Kumar, P., and Chandra, S. (2005). Comparative study on stone matrix asphalt mixes with different stablizers. In. (Eighty Fourth Annual Meeting 2005, Transporattaion Research Board….
- Kumar, R., Chandra, S.P., and Sharma, B.S. (2012). Giant intradiploic pseudomeningocele of occipital bone: case report. Journal of Neurosurgery: Pediatrics 9, 82-85.
- Kumar, S., Attrish, D., Srivastava, A., Banerjee, J., Tripathi, M., Chandra, P.S., and Dixit, A.B. (2021). Non-histone substrates of histone deacetylases as potential therapeutic targets in epilepsy. Expert Opinion on Therapeutic Targets.
- Kumar, S., Banerjee, J., Tripathi, M., Chandra, P.S., and Dixit, A.B. (2020). IDH1-R132H-FAT1-ROS-HIF-1α Signaling Pathway Inhibits Glioblastoma Tumor Progression. Neurology India 68, 1059.
- Kumar, S., Ramanujam, B., Chandra, P., Dash, D., Mehta, S., Anubha, S., Appukutan, R., Rana, M.K., and Tripathi, M. (2018). Randomized controlled study comparing the efficacy of rapid and slow withdrawal of antiepileptic drugs during long‐term video‐EEG monitoring. Epilepsia 59, 460-467.
- Kumar, V., Jain, S., Chandra, P., and Kumar, A. (2016). Management of postvitrectomy retinal detachment due to multiple laser-induced retinal holes. Case Reports 2016, bcr2016216887.
- Kumari, K., Sharma, M.C., Kakkar, A., Malgulwar, P.B., Pathak, P., Suri, V., Sarkar, C., Chandra, S.P., and Faruq, M. (2020). mTOR pathway activation in focal cortical dysplasia. Annals of diagnostic pathology 46, 151523.
- Kumari, K., Sharma, M.C., Kakkar, A., Malgulwar, P.B., Pathak, P., Suri, V., Sarkar, C., Chandra, S.P., Faruq, M., and Gupta, R.K. (2016). Role of mTOR signaling pathway in the pathogenesis of subependymal giant cell astrocytoma–A study of 28 cases. Neurology India 64, 988.
- Kumari, R., Kumar, S., Kasturi, S., Reddy, S., Chandra, S., Subbareddy, Madhan, G., Prakesh, Ramesh, and Kumar, V. (2017). GW28-e0117 Impact of Gene Polymorphisms, Platelet Reactivity, and the SYNTAX Score on 1-Year Clinical Outcomes in Patients with Acute Coronary Syndrome Undergoing Percutaneous Coronary Intervention. Journal of the American College of Cardiology 70, C91-C91.
- Kumawat, R., Gowda, S.H., Debnath, E., Rashid, S., Niwas, R., Gupta, Y., Upadaya, A.D., Suri, A., Chandra, P.S., and Gupta, D.K. (2018). Association of Single Nucleotide Polymorphisms (SNPs) in genes encoding for folate metabolising enzymes with glioma and meningioma in Indian population. Asian Pacific journal of cancer prevention: APJCP 19, 3415.
- Kurwale, N., Chandra, P.S., Tandon, V., Garg, A., Sarkar, C., Tripathi, M., Bal, C., and Tripathi, M. (2016). Use of multi-modal imaging to improve the localization of epileptogenic focus. International Journal of Epilepsy 3, A18.
- Kurwale, N., Chandra, P.S., Tandon, V., Garg, A., Sarkar, C., Tripathi, M., Bal, C., and Tripathi, M. (2016). Role of intraoperative MRI in epilepsy surgeries: Preliminary experience for two years. International Journal of Epilepsy 3, A17.
- Kurwale, N., Garg, K., Arora, A., Chandra, P.S., and Tripathi, M. (2016). Valproic acid as an antiepileptic drug: Is there a clinical relevance for the epilepsy surgeon? Epilepsy research 127, 191-194.
- Kurwale, N., Garg, K., Chandra, S., and Tripathi, M. (2014). VALPROATE ASSOCIATED COAGULOPATHY AND PLATELET DYSFUNCTION: CLINICAL RELEVANCE FOR EPILEPSY SURGEON: p323. Epilepsia 55.
- Kurwale, N.S., Chandra, S.P., Chouksey, P., Arora, A., Garg, A., Sarkar, C., Bal, C., and Tripathi, M. (2015). Impact of intraoperative MRI on outcomes in epilepsy surgery: preliminary experience of two years. British journal of neurosurgery 29, 380-385.
- Lee, B., Jeelani, Y., McComb, J.G., Alexiou, G.A., Garg, K., Chandra, P.S., Singh, P.K., Sharma, B.S., Kumar, R., and Pandey, A. (2013). Front & Back Matter. Pediatric Neurosurgery 49.
- Mahajan, C., Chouhan, R.S., Rath, G.P., Dash, H.H., Suri, A., Chandra, P.S., and Mahajan, A. (2014). Effect of intraoperative brain protection with propofol on postoperative cognition in patients undergoing temporary clipping during intracranial aneurysm surgery. Neurology India 62, 262.
- Majumdar, A., Kakkar, A., Kumar, A., Pathak, P., Sharma, M., Suri, V., Chandra, S., and Sarkar, C. (2016). GENOME-WIDE MICRORNA EXPRESSION PROFILE AND REGULATORY SIGNALING PATHWAYS IN GANGLIOGLIOMA. In EPILEPSIA. (WILEY 111 RIVER ST, HOBOKEN 07030-5774, NJ USA), pp 58-59.
- Malhotra, V., Chandra, S.P., Dash, D., Garg, A., Tripathi, M., Bal, C., and Tripathi, M. (2016). A screening tool to identify surgical candidates with drug refractory epilepsy in a resource limited settings. Epilepsy research 121, 14-20.
- Mandal, A., Singh, A., Stalin, C., Chandra, S., and Gandhi, P. (2018). Near Infrared JHKs observations of the transient MAXI J1820+ 070/ASASSN-18ey. The Astronomer's Telegram 11458, 1.
- Mankotia, D.S., Sardana, H., Sinha, S., Sharma, B.S., Suri, A., Borkar, S.A., Satyarthee, G.D., and Chandra, P.S. (2016). Pediatric interhemispheric arachnoid cyst: An institutional experience. Journal of pediatric neurosciences 11, 29.
- Mankotia, D.S., Sawarkar, D.P., Singh, P.K., Kumar, A., Verma, S.K., Chandra, P.S., and Kale, S.S. (2018). Rare case of cerebrospinal fluid proctorrhea caused by anterior sacral meningocele with rectothecal fistula. World neurosurgery 114, 323-325.
- Mathern, G.W., Andres, M., Salamon, N., Chandra, P.S., Andre, V.M., Cepeda, C., Levine, M.S., Leite, J.P., Neder, L., and Vinters, H.V. (2007). A hypothesis regarding the pathogenesis and epileptogenesis of pediatric cortical dysplasia and hemimegalencephaly based on MRI cerebral volumes and NeuN cortical cell densities. Epilepsia 48, 74-78.
- Mathern, G.W., and Chandra, S.P. (2006). Epilepsy surgery in children. MedLink Neurology.
- Meena, R., Doddamani, R., Agrawal, D., and Chandra, P. (2021). Dorsal Root Entry Zone (DREZ) Lesioning for Brachial Neuralgia (vol 68, pg 1012, 2020). NEUROLOGY INDIA 69, 236-236.
- Meena, R., Doddamani, R.S., Agrawal, D., and Chandra, P.S. (2020). Dorsal Root Entry Zone (DREZ) Lesioning for Brachial Neuralgia. Neurology India 68, 1012.
- Meena, R., Doddamani, R.S., Chipde, H., Agrawal, D., Mahajan, S., and Chandra, P. (2021). Management Dilemma in A Rare Case of Bilateral Temporo-Insular Glioma. Neurology India 69, 470.
- Meena, R.K., Doddamani, R.S., Chipde, H., Mahajan, S., Chandra, S.P., and Sawarkar, D.P. (2020). Primary spinal atypical teratoid/rhabdoid tumour presenting with hematomyelia and subarachnoid haemorrhage—a case report. Child's Nervous System 36, 655-659.
- Meena, R.K., Doddamani, R.S., Gurjar, H.K., Kumar, A., and Chandra, P.S. (2020). Type 1.5 split cord malformations: an uncommon entity. World neurosurgery 133, 142-149.
- Mehta, V., and Chandra, P. (2007). Tumors in Children. Pediatric Oncology (Surgical & Medical Aspects), 375.
- Mehta, V., Chandra, P., Singh, P.K., Garg, A., and Rath, G. (2009). Surgical considerations for'intrinsic'brainstem gliomas: Proposal of a modification in classification. Neurology India 57, 274.
- Mirpuri, P., Chandra, P.P., Samala, R., Agarwal, M., Doddamani, R., Kaur, K., Ramanujan, B., Chandra, P.S., and Tripathi, M. (2021). The development and efficacy of a mobile phone application to improve medication adherence for persons with epilepsy in limited resource settings: A preliminary study. Epilepsy & Behavior 116, 107794.
- Mishra, S., Chandra, P.S., Suri, A., Rajender, K., Sharma, B.S., and Mahapatra, A. (2010). Endoscopic management of third ventricular colloid cysts: eight years' institutional experience and description of a new technique. Neurology India 58, 412.
- Mishra, S., Singh, R., and Chandra, S. (1993). Prediction of subsidence in the Indo-gangetic basin carried by groundwater withdrawal. Engineering Geology 33, 227-239.
- Mohanty, A., Vasudev, M., and Chandra, P. (1998). Extradural haematoma complicating lumbar puncture following a craniotomy: A case report. Journal of neurosurgical sciences 42, 233.
- Mukherjee, S., Chandra, S., and Nayak, K. (1991). Studies on biochemical differences among isolates of Aeromonas hydrophila obtained from ulcerative disease affected fishes. In National Symposium on New Horizone in freshwater Aquaculture ICAR/CIFA, Bhubaneswar, India. pp 186-188.
- Mukherjee, S., Deepak, K., Yadav, R., Chandra, P., and Tripathi, M. (2004). Autonomic functions in patients with well-controlled and intractable epilepsy: a comparative study. In EPILEPSIA. (BLACKWELL PUBLISHING INC 350 MAIN ST, MALDEN, MA 02148 USA), pp 169-170.
- Mukherjee, S., Nagarsenkar, A., Chandra, S., and Sahasrabhojanee, M. (2013). Primary choriocarcinoma metastasizing to skeletal muscles, presenting as an abdominal wall mass: a rare presentation. Journal of natural science, biology, and medicine 4, 497.
- Mukherjee, S., Nagarsenkar, A., Chandra, S., Sahasrabhojanee, M., and Sawant, D. (2014). Amoebic cervicitis mimicking posterior wall fibroid: A rare presentation. Journal of Microbiology, Immunology and Infection 47, 354-357.
- Mukherjee, S., Tripathi, M., Chandra, P.S., Yadav, R., Choudhary, N., Sagar, R., Bhore, R., Pandey, R.M., and Deepak, K. (2009). Cardiovascular autonomic functions in well-controlled and intractable partial epilepsies. Epilepsy research 85, 261-269.
- Naik, V., Phalak, M., and Chandra, P.S. (2013). Total intracranial shunt migration. Journal of neurosciences in rural practice 4, 95.
- Nehra, A., Bajpai, S., Kale, S., Chandra, P., Tripathi, M., and Srivastava, A. (2016). Gamma knife versus open surgery for epilepsy: A longitudinal neuropsychological profiling study. International Journal of Epilepsy 3, A7.
- Nguyen, V., Serratosa, J., Gonzales, B., Genton, P., Michelucci, R., Sinha, S., Chandra, S., Beydoun, A., Arabi, M., and Kecmanovic, M. (2017). UPDATES TO THE LAFORA EPILEPSY CURE INITIATIVE (LECI) CLINICAL CENTER: DEVELOPMENT OF A DATA COLLECTION TOOL FOR MEASUREMENT OF LAFORA EPILEPSY DISEASE PROGRESSION. In EPILEPSIA. (WILEY 111 RIVER ST, HOBOKEN 07030-5774, NJ USA), pp S194-S195.
- Noufal Basheer, M., Chandra, P.S., and Mahapatra, A.K. Role of Decompressive Craniectomy for Malignant Middle Cerebral Artery Infarct: An Institutional Experience.
- Pandey, P., Chandra, P., Prasad, P., and Singh, S. (1977). Dipole moment derivatives from MINDO/3 semi-empirical MO calculations. Chemical Physics Letters 49, 353-356.
- Pandey, P., Tripathi, M., Chandra, P.S., Singh, V., and Mehta, V. (2001). Spontaneous decompression of a posterior fossa arachnoid cyst: a case report. Pediatric neurosurgery 35, 162-163.
- Parihar, J., Agrawal, M., Samala, R., Chandra, P.S., and Tripathi, M. (2020). Role of Neuromodulation for Treatment of Drug-Resistant Epilepsy. Neurology India 68, 249.
- Paul, D., Dixit, A., Srivastava, A., Tripathi, M., Tandon, V., Banerjee, J., and Chandra, P. (2016). ACTIVATION OF TRANSFORMING GROWTH FACTOR BETA (TGF beta) SIGNALLING IN MESIAL TEMPORAL LOBE EPILEPSY (MTLE) PATIENTS. In EPILEPSIA. (WILEY 111 RIVER ST, HOBOKEN 07030-5774, NJ USA), pp 151-151.
- Poodipedi, C.S., Tripathi, M., Singh, V.P., Bhatia, M., Kalra, V., and Mehta, V.S. (2002). II E13 Intractable epilepsy arising from a cerebellar hamartoma treated successfully by surgery: Case report. 日本てんかん学会プログラム・予稿集, 194.
- Prabhakar, H., Bindra, A., Chouhan, R., Chandra, P.S., and Tripathi, M. (2012). A54 Comparison of Effects of different Anaesthetic Techniques on Electrocorticography in Patients undergoing Epilepsy Surgery. European Journal of Anaesthesiology (EJA) 29, S16.
- Prasad, G.L., Kale, S.S., Mohanty, S.P., Sinha, S., and Chandra, P.S. (2017). Autologous Iliac Crest Bone Marrow Mononuclear Cells in Bone Fusion. Journal of Clinical & Diagnostic Research 11.
- Raheja, A., Agarwal, N., Mohapatra, S., Tandon, V., Borkar, S.A., Chandra, P.S., Kale, S.S., and Suri, A. (2020). Preparedness and guidelines for neurosurgery in the COVID-19 era: Indian perspective from a tertiary care referral hospital. Neurosurgical focus 49, E3.
- Raheja, A., Manjunath, N., Garg, K., Tandon, V., Gupta, V., Mishra, S., Ather, S., Suri, A., Chandra, P.S., and Singh, M. (2021). Turning a New Chapter in Neurosurgery Outpatient Services: Telemedicine A “Savior” in this Pandemic. Neurology India 69, 344.
- Raheja, A., Tandon, V., Suri, A., Chandra, P.S., Kale, S.S., Garg, A., Pandey, R.M., Kalaivani, M., Mahapatra, A.K., and Sharma, B.S. (2015). Initial experience of using high field strength intraoperative MRI for neurosurgical procedures. Journal of Clinical Neuroscience 22, 1326-1331.
- Raj, S., Snehi, S., Khan, M., Chandra, P., and Pandey, R. (2008). First molecular identification of a begomovirus associated with yellow vein net disease in grain amaranth (Amaranthus cruentus L.) in India. Australasian Plant Disease Notes 3, 129-131.
- Ramanujam, B., Bharti, K., Viswanathan, V., Garg, A., Tripathi, M., Bal, C., Chandra, P.S., and Tripathi, M. (2017). Can ictal-MEG obviate the need for phase II monitoring in people with drug-refractory epilepsy? A prospective observational study. Seizure 45, 17-23.
- Rath, G.P., Marda, M., Sokhal, N., Singh, P., and Chandra, P.S. (2010). Hypopharyngeal injury leading to subcutaneous emphysema after anterior cervical discectomy and artificial cervical disc placement. Journal of Clinical Neuroscience 17, 1447-1449.
- Rathore, Y.S., Chandra, P., Kumar, R., Singh, M., Sharma, M.S., Suri, A., Mishra, N., Gaikwad, S., Garg, A., and Sharma, B. (2012). Monitored gradual occlusion of the internal carotid artery followed by ligation for giant internal carotid artery aneurysms. Neurology India 60, 174.
- Ray, S., Tripathi, M., Chandra, S.P., and Chakravarty, K. (2017). Protocols in contemporary epilepsy surgery-a short communication. International journal of surgery (London, England) 44, 350-352.
- Rydenhag, B., Lindberg, I.O., and Malmgren, K. (2018). Surgery for drug-resistant epilepsy in children. The New England journal of medicine 378, 398-398.
- Salamon, N., Andres, M., Chute, D.J., Nguyen, S.T., Chang, J.W., Huynh, M.N., Chandra, P.S., Andre, V.M., Cepeda, C., and Levine, M.S. (2006). Contralateral hemimicrencephaly and clinical–pathological correlations in children with hemimegalencephaly. Brain 129, 352-365.
- Sanyal, S., Chandra, P., Tripathi, M., Singh, V., Padma, M., and Jain, S. (2005). Surgery for intractable post-traumatic epilepsy. In Epilepsia. (BLACKWELL PUBLISHING 9600 GARSINGTON RD, OXFORD OX4 2DQ, OXON, ENGLAND), pp 322-322.
- Sanyal, S.K., Chandra, P., and Tripathi, M. (2004). 739 The Intractable Epilepsy Problem in Developing Countries: Is There a Way Out? Neurosurgery 55, 465.
- Sanyal, S.K., Chandra, P.S., Gupta, S., Tripathi, M., Singh, V., Jain, S., Padma, M., and Mehta, V. (2005). Memory and intelligence outcome following surgery for intractable temporal lobe epilepsy: relationship to seizure outcome and evaluation using a customized neuropsychological battery. Epilepsy & Behavior 6, 147-155.
- Sarat Chandra, P., Jaiswal, A., and Mehta, V. (2003). Foramen magnum tumors: a series of 30 cases. Neurology India 51, 193.
- Sarkar, C., Sharma, M.C., Deb, P., Singh, V., Chandra, P.S., Gupta, A., Tripathi, M., Bhatia, M., Gaikwad, S., and Bal, C. (2006). Neuropathological spectrum of lesions associated with intractable epilepsies: A 10-year experience with a series of 153 resections. Neurology India 54, 144.
- Satyarthee, G.D., Chandra, P., and Mahapatra, A. (2017). Brain Studded with Innumerable Larger Stones: Starry Sky at Night Appearance: Multiple Calcified Giant Tuberculoma with 15 Years of Follow-up. Indian Journal of Neurosurgery 6, 155-158.
- Satyarthee, G.D., Chandra, P.S., Sharma, B.S., and Mehta, V. (2017). Comparison of stereotactic and ultrasound-guided biopsy of solid supratentorial tumor: a preliminary report. Asian journal of neurosurgery 12, 664.
- Sawarkar, D., Agrawal, M., Singh, P.K., Mishra, S., Agrawal, D., Kumar, A., Verma, S., Doddamani, R., Meena, R., and Garg, K. (2021). Evolution to Pedicle Reformation Technique in Surgical Management of Hangman's Fracture. World Neurosurgery.
- Sawarkar, D., Kumar, R., Singh, P., Agrawal, D., Sinha, S., Gupta, D., Satyarthee, G., Singh, M., Suri, A., and Chandra, P. (2017). Surgical outcome of microsurgical excision of brain and spinal cord cavernomas: Our 13 year single center experience. European Journal of Cancer 72, S47.
- Sebastiano, D.R., Tassi, L., Spreafico, R., and Panzica, F. (2020). Reply to" Maximizing non-invasive investigations in the quest for identifying the epileptogenic zone". Clinical neurophysiology: official journal of the International Federation of Clinical Neurophysiology 131, 2779-2780.
- Sharma, A., Damle, N., Tripathi, M., Saratchandra, P., and Bal, C. (2015). Role of SISCOS (Subtraction ictal SPECT coregistered to inter-ictal brain SPECT) in localization of epileptogenic foci in patients with structural defects on MRI. Journal of Nuclear Medicine 56, 1597-1597.
- Sharma, B.S., Ahmad, F.U., Chandra, P.S., and Mahapatra, A.K. (2008). Trigeminal schwannomas: experience with 68 cases. Journal of Clinical Neuroscience 15, 738-743.
- Sharma, B.S., and Chandra, P.S. (2002). 39 Neurocysticercosis: Neurosurgical Perspective. Taenia solium cysticercosis: from basic to clinical science, 387.
- Sharma, B.S., Kasliwal, M.K., Suri, A., Chandra, P.S., Gupta, A., and Mehta, V. (2010). Outcome following surgery for ophthalmic segment aneurysms. Journal of Clinical Neuroscience 17, 38-42.
- Sharma, D., Dixit, A., Banerjee, J., Tripathi, M., and Chandra, P. (2017). AN INTEGRATIVE ANALYSIS OF GENOME-WIDE PROFILING OF DNA METHYLATION AND GENE EXPRESSION IN FOCAL CORTICAL DYSPLASIA. In EPILEPSIA. (WILEY 111 RIVER ST, HOBOKEN 07030-5774, NJ USA), pp S89-S90.
- Sharma, D., Shrivastava, A., Dixit, B.A., Banerjee, J., Tripathi, M., and Chandra, P. (2016). GENE EXPRESSION ANALYSIS OF DRUG TRANSPORTERS AND BIOTRANSFORMATION ENZYME IN PATIENTS WITH MESIAL TEMPORAL LOBE EPILEPSY AND FOCAL CORTICAL DYSPLASIA: A COMPARATIVE STUDY. In EPILEPSIA. (WILEY 111 RIVER ST, HOBOKEN 07030-5774, NJ USA), pp 52-52.
- Sharma, D., Srivastava, A., Dixit, A.B., Banerjee, J., Tripathi, M., and Chandra, P.S. (2016). Gene expression analysis of drug transporters and biotransformation enzyme in patients with MTLE and FCD: A comparative study. International Journal of Epilepsy 3, A14.
- Sharma, M., Arora, R., Mahapatra, A., Sarat-Chandra, P., Gaikwad, S., and Sarkar, C. (2000). Intrasellar tuberculoma—an enigmatic pituitary infection: a series of 18 cases. Clinical neurology and neurosurgery 102, 72-77.
- Sharma, M., Chandra, P., and Gaur, R. (1983). Heydenia myrsines-new report from India. Indian Phytopathology (India).
- Sharma, M., Chandra, P.S., Goel, S., Gupta, V., and Sarkar, C. (2005). Primary lumbosacral Wilms tumor associated with diastematomyelia and occult spinal dysraphism. Child's Nervous System 21, 240-243.
- Sharma, M., Kumari, K., Kakkar, A., Sarkar, C., Suri, V., and Chandra, S. (2015). SG-02ROLE OF mTOR SIGNALLING PATHWAY IN THE PATHOGENESIS OF SUBEPENDYMAL GIANT CELL ASTROCYTOMAS. Neuro-oncology 17, iii35.
- Sharma, M.C., Jain, D., Gupta, A., Sarkar, C., Suri, V., Garg, A., Gaikwad, S., and Chandra, P.S. (2009). Dysembryoplastic neuroepithelial tumor: a clinicopathological study of 32 cases. Neurosurgical review 32, 161-170.
- Sharma, M.S., Suri, A., Chandra, S.P., Kale, S.S., Kapil, A., Sharma, B.S., and Mahapatra, A.K. (2012). Cost and usage patterns of antibiotics in a tertiary care neurosurgical unit. Indian Journal of Neurosurgery 1, 041-047.
- Sharma, M.S., Thapa, A., Chandra, S.P., Suri, A., Singh, M., Bahl, V.K., and Sharma, B.S. (2010). Intraoperative pulse and blood pressure recordings of neurosurgeons: a pilot study of cardiovascular performance. Neurosurgery 66, 893-899.
- Sharma, M.S., Vohra, A., Thomas, P., Kapil, A., Suri, A., Chandra, P.S., Kale, S.S., Mahapatra, A.K., and Sharma, B.S. (2009). EFFECT OF RISK‐STRATIFIED, PROTOCOL‐BASED PERIOPERATIVE CHEMOPROPHYLAXIS ON NOSOCOMIAL INFECTION RATES IN A SERIES OF 31 927 CONSECUTIVE NEUROSURGICAL PROCEDURES (1994–2006). Neurosurgery 64, 1123-1131.
- Sharma, R., Borkar, S., Katiyar, V., Goda, R., Phalak, M., Joseph, L., Suri, A., Chandra, P.S., and Kale, S.S. (2020). Interplay of dynamic extension reserve and T1 slope in determining the loss of cervical lordosis following laminoplasty: A novel classification system. World neurosurgery 136, e33-e40.
- Sharma, R., Garg, K., Agarwal, S., Agarwal, D., Chandra, P.S., Kale, S.S., Sharma, B.S., and Mahapatra, A.K. (2017). Microvascular decompression for hemifacial spasm: a systematic review of vascular pathology, long term treatment efficacy and safety. Neurology India 65, 493.
- Sharma, R., Garg, K., Katiyar, V., Tandon, V., Agarwal, D., Singh, M., Chandra, S.P., Suri, A., Kale, S.S., and Mahapatra, A.K. (2019). The role of mifepristone in the management of meningiomas: A systematic review of literature. Neurology India 67, 698.
- Sharma, R., Sharma, R., Tandon, V., Phalak, M., Garg, K., Singh, M., Gupta, D., Agrawal, D., Chandra, S.P., and Kale, S.S. (2020). Is Endoscopic Third Ventriculostomy a Feasible Option or Ventriculoperitoneal Shunt a Safer Bet for the Treatment of Posttraumatic Hydrocephalus? A Gap Time Model-based Algorithm. Neurology India 68, 1125.
- Sharma, S., Chandra, P.S., Abuzer, A., Suri, A., Gaikwad, S., Mishra, N., Dash, H., Sharma, B., and Mahapatra, A. (2012). Posterior circulation aneurysms: a 10-year institutional analysis. Indian Journal of Neurosurgery 1, 119-123.
- Shukla, G., Bhatia, M., Srivastava, M.P., Tripathi, M., Srivastava, A., Singh, V., Saratchandra, P., Gupta, A., Gaikwad, S., and Bal, C. (2005). Unidirectional whole body turning: a new lateralising sign in complex partial seizures. Journal of Neurology, Neurosurgery & Psychiatry 76, 1726-1729.
- Singh, J., Garg, K., Satyarthee, G., Chandra, P., and Singh, M. (2021). Dynamic MRI in Cervical Myelopathy: A Useful Tool? Neurology India 69, 211-211.
- Singh, K., Sharma, R., Sharma, A., and Chandra, S. (2012). Biodegradating fungal flora isolated from petroleum contaminated soil in rural area of Jaipur Distict, Rajasthan (India). CIBTech Journal of Biotechnology 1, 3.
- Singh, M., Chandra, P., and Sharma, B. (2013). Aggressive surgical management of craniopharyngiomas. Indian Journal of Neurosurgery 2, 138-141.
- Singh, M., and CHANDRA, S. (1971). Occurrence of. Platypepla aprobola.
- Singh, P., Chandra, P., Kale, S., Sawarkar, D., Kumar, A., and Verma, S. (2018). Long Term Surgical Outcome of Paediatric Vertebral Haemangiomas Presenting with Myelopathy. In PEDIATRIC BLOOD & CANCER. (WILEY 111 RIVER ST, HOBOKEN 07030-5774, NJ USA), pp S316-S316.
- Singh, P., Chandra, P., Kale, S., Sharma, B., Mahapatra, A., and Sawarker, D. (2017). MANAGEMENT OF PAEDIATRIC VERTEBRAL HAEMANGIOMAS PRESENTING WITH MYELOPATHY WITH MINIMUM 2-YEAR FOLLOW UP. In OSTEOPOROSIS INTERNATIONAL. (SPRINGER LONDON LTD 236 GRAYS INN RD, 6TH FLOOR, LONDON WC1X 8HL, ENGLAND), pp S129-S129.
- Singh, P., Chandra, P., Sawarkar, D., Kale, S., Sharma, B., and Kumar, A. (2017). Management of symptomatic paediatric vertebral haemangiomas by an innovative technique. European Journal of Cancer 1, S47.
- Singh, P., Chandra, P.S., Kale, S., Verma, S., Sawarkar, D., and Kumar, A. (2018). NSRG-10. SURGICAL MANAGEMENT OF SYMPTOMATIC PAEDIATRIC VERTEBRAL HAEMANGIOMAS PRESENTING WITH MYELOPATHY WITH LONG TERM FOLLOW UP. Neuro-oncology 20, i147.
- Singh, P., Chandra, S., and Kale, S. (2020). Management of Symptomatic Paediatric Vertebral Haemangiomas by Innovative Technique in Resource Constrained Setting. In PEDIATRIC BLOOD & CANCER. (WILEY 111 RIVER ST, HOBOKEN 07030-5774, NJ USA), pp S321-S321.
- Singh, P., Josef, S., Chandra, S., and Kale, S. (2020). MANAGEMENT OF PEDIATRIC BASILAR ARTERY ANEURYSMS. In INTERNATIONAL JOURNAL OF STROKE. (SAGE PUBLICATIONS LTD 1 OLIVERS YARD, 55 CITY ROAD, LONDON EC1Y 1SP, ENGLAND), pp 581-582.
- Singh, P., Mishra, N.K., Dash, H.H., Thyalling, R.K., Sharma, B.S., Sarkar, C., and Chandra, P.S. (2011). Treatment of vertebral hemangiomas with absolute alcohol (ethanol) embolization, cord decompression, and single level instrumentation: a pilot study. Neurosurgery 68, 78-84.
- Singh, P., Sarkari, A., Chandra, P.S., Mahapatra, A., Sharma, B., and Gurjar, H. (2012). Giant craniopharyngioma presenting as a cerebellopontine angle tumour. Pediatric neurosurgery 48, 131.
- Singh, P., Sawarkar, D., Chandra, P.S., Kale, S., and Sharma, B.S. (2016). NS-07MANAGEMENT OF PAEDIATRIC SINGLE LEVEL VERTEBRAL HEMANGIOMAS PRESENTING WITH MYELOPATHY WITH MORE THAN ONE YEAR FOLLOWUP. Neuro-Oncology 18, iii128.
- Singh, P., Sawarkar, D., Kumar, A., Verma, S., Agarwal, D., Chandra, S., and Kale, S. (2018). MANAGEMENT OF PEDIATRIC AXIS FRACTURES: AN INSTITUTIONAL EXPERIENCE. In OSTEOPOROSIS INTERNATIONAL. (SPRINGER LONDON LTD 236 GRAYS INN RD, 6TH FLOOR, LONDON WC1X 8HL, ENGLAND), pp S219-S219.
- Singh, P., Singla, R., Chandra, P., Kale, S., and Mahapatra, A. (2017). RARE-34. AN INSTITUTIONAL REVIEW OF NINE CASES OF SPINAL HEMANGIOPERICYTOMA. Neuro-oncology 19, vi217.
- Singh, P., Verma, S., Sawarkar, D., Kumar, A., Agarwal, D., Chandra, P., and Kale, S. (2018). Evolution in the Management of Combined Atlas—Hangman's Fracture. Journal of Neurological Surgery Part A: Central European Neurosurgery 79, P28.
- Singh, P.K., Agrawal, M., Mishra, S., Agrawal, D., Sawarkar, D., Jagdevan, A., Verma, S., Doddamani, R., Meena, R., and Garg, K. (2020). Management of C2 Body Giant Cell Tumor by Innovatively Fashioned Iliac Crest Graft and Modified Cervical Mesh Cage Used as Plate. World Neurosurgery 140, 241-246.
- Singh, P.K., Agrawal, M., Sawarkar, D., Kumar, A., Verma, S., Doddamani, R., Chandra, P.S., and Kale, S.S. (2020). Management of neglected complex hangman’s fracture by reforming the C2 pedicle: new innovative technique of motion preservation at the C1–2 joint in 2 cases. Journal of Neurosurgery: Spine 32, 965-972.
- Singh, P.K., and Chandra, P. (2012). Early Versus Delayed Endoscopic Surgery for Carpal Tunnel Syndrome: A Prospective Study. In JOURNAL OF NEUROSURGERY. (AMER ASSOC NEUROLOGICAL SURGEONS 5550 MEADOWBROOK DRIVE, ROLLING MEADOWS, IL…), pp A439-A439.
- Singh, P.K., Chandra, P.S., Vaghani, G., Savarkar, D.P., Garg, K., Kumar, R., Kale, S.S., and Sharma, B.S. (2016). Management of pediatric single-level vertebral hemangiomas presenting with myelopathy by three-pronged approach (ethanol embolization, laminectomy, and instrumentation): a single-institute experience. Child's Nervous System 32, 307-314.
- Singh, P.K., Chandra, S.P., Agrawal, M., Sawarkar, D., Kumar, R., Garg, A., Kumar, A., Verma, S., Doddamani, R., and Meena, R. Surgery for Vertebral Hemangioma in Resource-Constrained Environment. Available at SSRN 3782453.
- Singh, P.K., Chandra, S.P., Agrawal, M., Sawarkar, D., Kumar, R., Kumar, A., Verma, S., and Kale, S.S. (2020). Long-Term Outcome of Surgical Management in Symptomatic Pediatric Vertebral Hemangiomas Presenting With Myelopathy. Neurosurgery 87, 1240-1251.
- Singh, P.K., Verma, S.K., Garg, M., Sawarkar, D.P., Kumar, A., Agrawal, D., Chandra, S.P., Kale, S.S., Sharma, B.S., and Mahapatra, A.K. (2017). Evaluation of Correction of Radiologic Parameters (Angulation and Displacement) and Accuracy of C2 Pedicle Screw Placement in Unstable Hangman's Fracture with Intraoperative Computed Tomography–Based Navigation. World neurosurgery 107, 795-802.
- Singh, R., Tasnim, S., Chandra, S., Suri, A., and BhattacharjeeJ, T.S. (2021). Association of NF-κB with Recurrence of Myocardial Infarction-A Study in North Indian Population. J Cardiol Cardiovasc Res 2, 1-7.
- Singh, V., Chaudhary, K., Kumaran, S.S., Chandra, S., and Tripathi, M. (2020). Functional Cerebral Specialization and Decision Making in the Iowa Gambling Task: A Single-Case Study of Left-Hemispheric Atrophy and Hemispherotomy. Frontiers in psychology 11.
- Singla, R., Singh, P.K., Khanna, G., Suri, V., Agarwal, D., Chandra, P., Kale, S., and Mahapatra, A. (2020). an institutional review of 10 cases of spinal hemangiopericytoma/solitary fibrous tumor. Neurology India 68, 448.
- Sinha, S., Kale, S.S., Chandra, S.P., Suri, A., Mehta, V.S., and Sharma, B.S. (2014). Brainstem gliomas: surgical indications and technical considerations in a series of 58 cases. British journal of neurosurgery 28, 220-225.
- Sinha, V., Chandra, P., Kumar, V., and Sarkar, C. (2015). The Impact of Post Harvest Agricultural Crop Residue Fires on Volatile Organic Compounds and Formation of Secondary Air Pollutants in the NW Indo-Gangetic Plain. In AGU Fall Meeting Abstracts. pp A21A-0037.
- Sokhal, N., Rath, G.P., Chaturvedi, A., Dash, H.H., Bithal, P.K., and Chandra, P.S. (2015). Anaesthesia for awake craniotomy: A retrospective study of 54 cases. Indian journal of anaesthesia 59, 300.
- Soni, D., Dhawan, S., Agarwal, S., Chandra, N., Chandra, P., Dwivedi, S., Puri, V., and Hasan, M. (1991). Clinical relevance of vegetations in infective endocarditis. Indian heart journal 43, 373-376.
- Sreenivasan, R., Sharma, R., Borkar, S.A., Arumulla, S., Garg, K., Chandra, S.P., Kale, S.S., and Mahapatra, A.K. (2020). Cervical Split Cord Malformations: A Systematic Review. Neurology India 68, 994.
- Sreenivasan, S.A., Garg, K., Mishra, S., Singh, P.K., Singh, M., and Chandra, P.S. (2018). Letter to the Editor. Local steroid application during anterior cervical discectomy and fusion. Journal of Neurosurgery: Spine 30, 296-297.
- Sreenivasan, S.A., Garg, K., Nambirajan, A., Suri, V., Singh, M., and Chandra, P.S. (2019). Rosette-forming glioneuronal tumour of dorsolumbar spinal cord. Child's Nervous System 35, 1277-1279.
- Sreenivasan, S.A., Garg, K., Singh, M., and Chandra, P.S. (2018). Letter to the Editor. Cervical intramedullary tumor resection and kyphotic malalignment. Journal of Neurosurgery: Spine 29, 348-350.
- Srinivasa, K., Chandra, S., Kajaria, S., and Mukherjee, S. (2011). IGIDS: Intelligent intrusion detection system using genetic algorithms. In 2011 World Congress on Information and Communication Technologies. (IEEE), pp 852-857.
- Srivastava, A., Banerjee, J., Dubey, V., Tripathi, M., Chandra, P.S., Sharma, M., Lalwani, S., Siraj, F., Doddamani, R., and Dixit, A.B. (2020). Role of Altered Expression, Activity and Sub-cellular Distribution of Various Histone Deacetylases (HDACs) in Mesial Temporal Lobe Epilepsy with Hippocampal Sclerosis. Cellular and Molecular Neurobiology, 1-16.
- Srivastava, A., Dixit, A., Dodamanni, R., Banerjee, J., Thipathi, M., and Chandra, P.S. (2018). Expression Profile of Histone Deacetylases in Patients with Hippocampal Sclerosis. International Journal of Epilepsy 5, A0005.
- Srivastava, A., Dixit, A.B., Banerjee, J., Tripathi, M., and Chandra, P.S. (2016). Role of inflammation and its miRNA based regulation in epilepsy: Implications for therapy. Clinica Chimica Acta 452, 1-9.
- Srivastava, A., Dixit, A.B., Paul, D., Tripathi, M., Sarkar, C., Chandra, P.S., and Banerjee, J. (2017). Comparative analysis of cytokine/chemokine regulatory networks in patients with hippocampal sclerosis (HS) and focal cortical dysplasia (FCD). Scientific reports 7, 1-11.
- Srivastava, S., Bhatia, M., and Chandra, S. (2015). North Zone: A voxel based DTI study showing white matter abnormalities in first episode, treatment naive patients of depressive disorder. In INDIAN JOURNAL OF PSYCHIATRY. (WOLTERS KLUWER MEDKNOW PUBLICATIONS WOLTERS KLUWER INDIA PVT LTD, A-202, 2ND…), pp S10-S10.
- Suri, A., Bansal, S., Sharma, B., Mahapatra, A.K., Kale, S.S., Chandra, S.P., Singh, M., Kumar, R., and Sharma, M. (2012). Hypoglossal schwannomas: Single institutional experience of 14 cases. Journal of Neurological Surgery Part B: Skull Base 73, A129.
- Suri, A., Bansal, S., Sharma, B.S., Mahapatra, A.K., Kale, S.S., Chandra, P.S., Singh, M., Kumar, R., and Sharma, M.S. (2014). Management of hypoglossal schwannomas: single institutional experience of 14 cases. Journal of neurological surgery Part B, Skull base 75, 159.
- Suri, A., Kale, S., Chandra, P., Chabbra, R., Mahapatra, A., and Mehta, V. (2002). Developmental osseous craniovertebral junction anomalies: Dilemmas and controversies. In NEUROSURGERY. (LIPPINCOTT WILLIAMS & WILKINS 530 WALNUT ST, PHILADELPHIA, PA 19106-3621 USA), pp 543-543.
- Swami, P., Bhatia, M., Tripathi, M., Chandra, P.S., Panigrahi, B.K., and Gandhi, T.K. (2019). Selection of optimum frequency bands for detection of epileptiform patterns. Healthcare technology letters 6, 126-131.
- Tandon, V., Bansal, S., Chandra, P.S., Suri, A., Tripathi, M., Sharma, M.C., Sarkari, A., and Mahapatra, A.K. (2016). Ganglioglioma: Single-institutional experience of 24 cases with review of literature. Asian journal of neurosurgery 11, 407.
- Tandon, V., Chandra, P.S., Doddamani, R.S., Subianto, H., Bajaj, J., Garg, A., and Tripathi, M. (2018). Stereotactic radiofrequency thermocoagulation of hypothalamic hamartoma using robotic guidance (ROSA) coregistered with O-arm guidance—preliminary technical note. World neurosurgery 112, 267-274.
- Tandon, V., Chandra, P.S., Singla, R., Bajaj, J., Kakkar, A., Sharma, M.C., Mahapatra, A.K., and Tripathi, M. (2019). Drug Refractory Epilepsy–A Series of Lesions with Triple Pathology. Neurology India 67, 1093.
- Tandon, V., Lang, M., Chandra, P.S., Sharan, A., Garg, A., and Tripathi, M. (2018). Is edema a matter of concern after laser ablation of epileptogenic focus? World neurosurgery 113, 366-372. e363.
- Tandon, V., Raheja, A., Mishra, S., Garg, K., Dash, C., Borkar, S.A., Wellington, J., Chaurasia, B., Fontanella, M.M., and Suri, A. (2021). Trends in neurosurgical teleconsultation services across the globe during COVID-19 pandemic. World Neurosurgery.
- Tandon, V., Raheja, A., Suri, A., Chandra, P.S., Kale, S.S., Kumar, R., Garg, A., Kalaivani, M., Pandey, R.M., and Sharma, B.S. (2017). Randomized trial for superiority of high field strength intra-operative magnetic resonance imaging guided resection in pituitary surgery. Journal of Clinical Neuroscience 37, 96-103.
- Thakur, N., Tandon, V., and Chandra, P.S. (2012). Modification of Penfield dissector as monopolar cautery point for transoral odontoidectomy. Indian Journal of Neurosurgery 1, 089-089.
- Thakur, R., Mathur, K., Rao, V., Chandra, S., Shivramkrishnan, S., Kannan, S., Hiremath, R., Tailor, H., Kushwaha, U., and Dwivedi, R. (1998). Pathogenic and genetic characterization of six Indian populations of Colletotrichum sublineolum, the causal agent of sorghum anthracnose. Indian Phytopathology 51, 338-348.
- Thapa, A., Chandra, P.S., Sinha, S., Gupta, A., Singh, M., Suri, A., and Sharma, B. (2009). Surgical interventions in intracranial arteriovenous malformations: Indications and outcome analysis in a changing scenario. Neurology India 57, 749.
- Thapa, A., Chandra, S.P., Sinha, S., Sreenivas, V., Sharma, B.S., and Tripathi, M. (2010). Post-traumatic seizures—a prospective study from a tertiary level trauma center in a developing country. Seizure 19, 211-216.
- TRIPATHI, I., CHANDRA, S., and SINGH, M. (1986). Triple test cross analysis in F2 populations of two barley crosses. International journal of tropical agriculture 4, 351-359.
- 427. Tripathi, M., Aggarwal, V., Singh, P., Goel, M., Garg, A., Bal, C., Gaikwad, S., Sarkar, C., Madakasira, P., and Singh, M. (2011). CORRELATION OF INTERICTAL SPIKES, ICTAL ONSET PATTERN, PROPAGATION TIME AND POSTOPERATIVE DISCHARGES WITH OUTCOME IN PERSONS UNDERGOING EPILEPSY SURGERY: p618. Epilepsia 52, 190-191.
- Tripathi, M., Chandra, S., Madakasira, P., Singh, M., Shukla, G., Gaikwad, S., Bal, C., and Sarkar, C. (2004). CONCORDANCE OF INTERICTAL EEG, LONG-TERM ICTAL VIDEO EEG, MRI, AND INTERICTAL SPECT AND HISTOPATHOLOGY WITH OUTCOME IN PATIENTS OPERATED ON FOR INTRACTABLE EPILEPSY: 2.445. Epilepsia 45.
- Tripathi, M., Chandra, S., Vani, K., Mukherjee, S., and Deepak, K. (2009). EFFECT OF TEMPORAL LOBE SURGERY ON CARDIOVASCULAR AUTONOMIC RESPONSES IN EPILEPTIC PATIENTS: E754. Epilepsia 50.
- Tripathi, M., Choudhary, N., Chandra, P., and Deepak, K. (2009). PO18-WE-53 Effect of temporal lobe epilepsy surgery on cardiovascular autonomic functions. Journal of the Neurological Sciences, S258.
- 431. Tripathi, M., Dixit, A., and Chandra, P.S. (2016). Galectin-3, an important yet unexplored molecule in drug resistant epilepsy. Neurology India 64, 237.
- 432. Tripathi, M., Garg, A., Bal, C., and Chandra, S. (2015). FDG-PET AND MRI COREGISTRATION IN MRI-SUBSTRATE NEGATIVE REFRATORY EPILEPSY: p0935. Epilepsia 56.
- 433. Tripathi, M., Garg, A., Gaikwad, S., Bal, C., Chitra, S., Prasad, K., Dash, H., Sharma, B., and Chandra, P.S. (2010). Intra-operative electrocorticography in lesional epilepsy. Epilepsy research 89, 133-141.
- 434. Tripathi, M., Goel, M., Bhatia, M., Jain, S., Padama, M., Gaikwad, S., Bal, C., Singh, V., Chandra, P., and Srivastava, A. (2003). Concordance of Interictal EEG, Ictal Video EEG, MRI AND Interictal SPECT with Histopathology in Patients Operated for Intractable Epilepsy in a Tertiary Referral Hospital in Northern India. Epilepsia 44, 61-62.
- Tripathi, M., Goel, V., Padma, M., Jain, S., Maheshwari, M., Gaikwad, S., Gupta, V., Chandra, P., and Mehta, V. (2003). Fenestration of the posterior communicating artery. Neurology India 51, 75.
- Tripathi, M., Jain, D., Devi, M.G., Jain, S., Saxena, V., Chandra, P., Radhakrishnan, K., Behari, M., Gupta, M., and Puri, V. (2012). Need for a national epilepsy control program. Annals of Indian Academy of Neurology 15, 89.
- Tripathi, M., Luthra, K., Chandra, S., Padma, V., and Singh, M. (2004). Federal de Santa Catarina, Florian@ olis/SC, Brasil," 2Hospital Santa Teresa, Sdo Pedro de Aledntara/SC, Brasil," 3Hospital Universitdrio/UFSC, Florian@ olis/SC, Brasil; 4Clinica Interdisciplinar de Epilepsia do Estado de SC, Florian@ olis/SC, Brasil; 5Centro de Controle de Intoxicaedes de Sdo Paulo, Brasil.
- Tripathi, M., Luthra, K., Chandra, S., Padma, V., Singh, M., and Srivastava, A. (2005). Apolipoprotein-e levels in intractable epileptics: In an Indian population. In JOURNAL OF THE NEUROLOGICAL SCIENCES. (ELSEVIER SCIENCE BV PO BOX 211, 1000 AE AMSTERDAM, NETHERLANDS), pp S147-S148.
- Tripathi, M., Luthra, K., Chandra, S., Padma, V., Singh, N., and Srivastava, A. (2005). Psychosocial and treatment seeking behaviour in patients with Epilepsy presenting to a tertiary care center in northern India. In JOURNAL OF THE NEUROLOGICAL SCIENCES. (ELSEVIER SCIENCE BV PO BOX 211, 1000 AE AMSTERDAM, NETHERLANDS), pp S147-S147.
- Tripathi, M., Padhy, U.P., Vibha, D., Bhatia, R., Srivastava, M.P., Singh, M.B., Prasad, K., and Chandra, S.P. (2011). Predictors of refractory epilepsy in North India: A case–control study. Seizure 20, 779-783.
- Tripathi, M., Padma, V., Bhatia, R., Prasad, K., and Chandra, S. (2008). MANAGEMENT OF REFRACTORY STATUS EPILEPTICUS IN PATIENTS PRESENTING TO A TERTIARY CARE CENTRE IN A DEVELOPING COUNTRY: 1.267. Epilepsia 49.
- Tripathi, M., Padma, V., Chandra, S., Mehta, S., and Bhavya, G. (2013). SEIZURE PHENEMENOLOGY INFERRED FROM CLINICAL DESCRIPTORS OF CAREGIVERS AND ITS CONCORDANCE TO ONLY VIDEO AND VIDEO-EEG RECORDINGS: 062. Epilepsia 54.
- Tripathi, M., Ray, S., and Chandra, P.S. (2016). Presurgical evaluation for drug refractory epilepsy. International Journal of Surgery 36, 405-410.
- Tripathi, M., Santosh, V., Nagaraj, D., Cristhopher, R., Chandra, P., and Shankar, S. (2001). Stroke in a young man with fibromuscular dysplasia of the cranial vessels with anticardiolipin antibodies: a case report. Neurological Sciences 22, 31-35.
- Tripathi, M., Singh, M., Madakasira, P., Gaikwad, S., Srivastava, A., Bal, C., Sarkar, C., and Chandra, S. (2007). PREDICTORS OF INTRACTABLE EPILEPSY: A REVIEW OF 254 INTRACTABLE EPILEPSY PATIENTS OPERATED AT A TERTIARY CARE CENTRE IN NORTHERN INDIA. p287. Epilepsia 48.
- Tripathi, M., Singh, M.S., Padma, M., Gaikwad, S., Bal, C., Tripathi, M., Sarkar, C., Gupta, A., Shukla, G., and Singh, V. (2008). Surgical outcome of cortical dysplasias presenting with chronic intractable epilepsy: A 10-year experience. Neurology India 56, 138.
- Tripathi, M., Vibha, D., Choudhary, N., Prasad, K., Srivastava, M.P., Bhatia, R., and Chandra, S.P. (2010). Management of refractory status epilepticus at a tertiary care centre in a developing country. Seizure 19, 109-111.
- Vaid, A., Patil, C., Sanghariyat, A., Rane, R., Visani, A., Mukherjee, S., Joseph, A., Ranjan, M., Augustine, S., and Sooraj, K. (2020). Emerging Advanced Technologies Developed by IPR for Bio Medical Applications‑. A Review. Neurology India 68, 26.
- Vamsi, K., Chandra, P.S., Sharma, B., and Mohapatra, A. (2010). Anterior sacral meningocele wrongly diagnosed as ovarian cyst. Pediatric neurosurgery 46, 245.
- Venkatesh, M., Chandra, S., and Singh, A. (1977). Susceptibility of F1 progeny of the field populations of the desert locust (Schistocerca gregaria Forsk.) surviving treatment with organochlorine insecticides. Journal of entomological research.
- Verma, S.K., Dharanipathy, S., Suri, A., Chandra, P.S., and Kale, S.S. (2020). Video Section-Operative Nuances: Step by Step–Donning and Doffing in Neurosurgical Operating Room. Neurology India 68, 796.
- Verma, S.K., Singh, P.K., Sawarkar, D.P., Kumar, A., Agarwal, D., Chandra, P.S., and Kale, S.S. (2019). Motion Preserving Surgery Using O-Arm for Unstable Hangman Fracture. Indian Journal of Neurotrauma 16, 02-09.
- Verma, S.K., Sinha, S., Sawarkar, D.P., Singh, P.K., Gupta, D., Agarwal, D., Satyarthee, G., Kumar, R., Singh, M., and Suri, A. (2016). Medial sphenoid wing meningiomas: Experience with microsurgical resection over 5 years and a review of literature. Neurology India 64, 465.
- Vinod, M., Shaw, S.C., Devgan, A., and Mukherjee, S. (2018). The currarino triad. Medical Journal, Armed Forces India 74, 374.
- Viswanathan, K.V., Bharti, K., Bhargavi, R., Chandra, P.S., Ajay, G., Madhavi, T., Chandrashekar, B., and Tripathi, M. (2016). Magnetoencephalographic (MEG) yield of single and multiple dipole clusters in patients with drug refractory epilepsy (DRE). International Journal of Epilepsy 3, A45.
- Wnuk, E., Maj, E., Dziedzic, T., and Piętowska, A.P. (2020). Spinal Epidural Venous Plexus Enlargement as a Cause of Neurologic Symptoms: Vascular Anatomy and MRI Findings. Neurology India 68, 1238.
- Yadav, N., Banerjee, J., Tripathi, M., Chandra, P., and Dixit, A. (2020). Association of Genetic Polymorphisms in Tumor Necrosis Factor-Alpha gene with the risk of Intracerebral Hemorrhage in North Indian Population. Neurology India 68, 84-85.
- Yadav, S., Rajput, S., Tripathi, M., Yadav, R., Chandra, S., and Singh, R. (2016). Effect of front line demonstration for enhancing the yield of chickpea (Cicer arietinum L.). Agriculture Update 11, 22-25.
- Yelamarthy, P.K., Chhabra, H., Vaccaro, A., Vishwakarma, G., Kluger, P., Nanda, A., Abel, R., Tan, W.F., Gardner, B., and Chandra, P.S. (2019). Management and prognosis of acute traumatic cervical central cord syndrome: systematic review and Spinal Cord Society—Spine Trauma Study Group position statement. European Spine Journal 28, 2390-2407.
- Yelamarthy, P.K., Chhabra, H., Vaccaro, A., Vishwakarma, G., Kluger, P., Nanda, A., Abel, R., Tan, W.F., Gardner, B., and Chandra, P.S. (2020). Correction to: Management and prognosis of acute traumatic cervical central cord syndrome: systematic review and Spinal Cord Society-Spine Trauma Study Group position statement. European spine journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society.
- Yerramneni, V.K., Chandra, P.S., Kale, S.S., Lythalling, R.K., and Mahapatra, A.K. (2011). A 6-year experience of 100 cases of pediatric bony craniovertebral junction abnormalities: treatment and outcomes. Pediatric neurosurgery 47, 45-50.
- Yerramneni, V.K., Chandra, P.S., Kasliwal, M.K., Sinha, S., Suri, A., Gupta, A., and Sharma, B.S. (2010). Recovery of oculomotor nerve palsy following surgical clipping of posterior communicating artery aneurysms. Neurology India 58, 103.
30 publications still pending to be udated
All the information mentioned above is correct to the best of my information
P Sarat Chandra

Prof.
A K Banerji
Others
Affiliation
Emeritus Professor
Department of
Neurosurgery
Contact
Email :
akb1935@yahoo.com
“It was May 1965 that I came to Delhi from Vellore where I was a lecturer, to appear for a Union Public Service Commission interview for the job of Reader at G. B. Pant hospital, Delhi and All India Institute of Mental Health, Bangalore (later to become NIMHANS). I was the only candidate and was asked at the end as to which place would I prefer. I chose Bangalore. Just before leaving for the interview, I had gone to see Dr. Baldev Singh and Dr P. N. Tandon (PNT) at AIIMS to pay a courtesy call. They were sharing an office and I suspect eagerly waiting like spiders, to catch a victim in neurosurgery, who could stick on at AIIMS, which at that time had actually nothing no space, equipment or staff. After a little talking about general things, suddenly, Dr. Baldev Singh asked me to think whether I at all wanted to go for the interview, as AIIMS could possibly offer me a job, I of course declined the proposal as a bird in hand was better than two in the bush. Then Dr. Tandon asked me to come home for tea that evening. I left for the Union Public Service Commission office. Today when I see large number of candidates for a job interview my own experience seems miraculous.
Coming back after the interview I recounted what happened to Gopal and his wife Radha (Dr. G.K. Vishwakarma was then Asst. Professor Orthopaedics and later became D.G.H.S. of Government of India) Insidious pressure started from them to come to AIIMS and forget about Bangalore. Incidentally Bangalore had a working, full fledged department with Prof. RM. Verma and he tried hard to get me there even after I joined AIIMS.
That evening I spent at Tandons. Dr. P. N. Tandon had been my Anatomy demonstrator in 1952 while Mrs. Leela Tandon was my lecturer in Obstetrics and Gynaecology at Medical College, Lucknow. I had met Dr. P.N. Tandon in 1963 at the annual Neurological Society of India meeting in Calcutta. For both of us it was the very first meeting that we had attended of NSI. Dr. P. N. Tandon had established the department of neurosurgery at AlIMS 2 months before in March 65. He had been promised equipment but nothing had arrived in the two months. He was eager that I should join but was frank to say he did not know how things would eventually develop. After returning to Gopal's house, Radha and Gopal took me to see 'My Fair Lady' at Sheila Theatre which then was the best in Delhi, if not India. After returning well past midnight we slept on the roof and went on talking about what I should do. I think it was near the break of dawn that I finally succumbed to pressures from Gopal and Radha and said OK I'll come to Delhi if the job was offered. Next morning before I left Delhi Dr. Baldev Singh took me to meet Prof. K. L. Wig then Director AIIMS. Our liking for each other was instantaneous and the bond carried throughout.
I joined as adhoc Assistant Professor in June'65. There was one office of Dr. Baldev Singh in which in addition to Dr. P. N. Tandon another chair and a small table was put for me. The process of starting a department began really from scratch. Space was allotted on the first floor by the side of anatomy lecture theatre. I and Dr. V. Virmani (my opposite number in Neurology) sat down to draw maps and carve out rooms in the large halls. At that moment, our vibes were bristly to say the least. Dr. Virmani was considerably senior in age plus she had known Dr. Baldev Singh since Amritsar days and she also held the trump card of being Punjabi speaking which was then the lingua franca of AIIMS. Over the years our relationship mellowed and we did develop mutual admiration and respect for each other. I hit upon the strategy in our dealings at that time of building the departments, of saying exactly opposite of what I wanted. Dr. Virmani would of course, reverse my suggestions much to my advantage. Today when I look back it all appears so childish. But then it was great fun. Slowly collecting items like pins, chairs, tables, almirahs and make real offices was a new challenge for which I was not trained. Anyway we built the office cubicles, laboratories and got the OPD on the 4th floor in ship shape. It was so gratifying after two years of joining that we had a place of our own.
We started with surgical instruments which actually were of World War II vintage which included an operation table. Burr holes had to be made by a brace in 4 stages and both Dr. Tandon and I developed the art to perfection. To begin with we had no beds. Both for Neurology and Neurosurgery, Prof. K.L. Wig and the Pediatricians generously allowed us use of their beds in what is now the nurses hostel. There was so little clinical work that it was terribly frustrating in the beginning. I started taking clinics for the MD students of medicine, pediatrics and radiology. I slowly became quite popular to the extent that one day Dr. Wig called me to see one of his patients in his office. I must have impressed him no end as after that on several occasions he would ask for my opinion on patients. This was a small matter for him but a great boost for my confidence for which my gratitude goes to him.
By 1968 we were having a ward in the OPD block (ward IX) and we were well settled. The operation theaters were in the College of Nursing Block. Radiology to begin with was in the nurses hostel, and only in 1968 shifted to its present location. That was the time when we had Dr. S. K. Ghosh in radiology from 1965 to 1968 and he was a great help. Very often we started the day at 7.30 A.M. with ward rounds, dressings and stitch removals, followed by neuroradiology (ventriculograms angiograms etc) and then this was followed by surgery which would invariably end by 7 or 8 P.M., particularly if it was a posterior fossa tumour. At night one of us i.e. PNT or myself would sleep in the doctors room adjacent to the main O.T. block. From 1966 onwards Dr. B.B. Sawhney and Dr. M. Gourie Devi, now Director and Vice Chancellor NIMHANS who were residents in neurology would help us out by doing night duties and also assist in surgery as we did not have regular residents of our own. The role played by Col. G.C. Tandon, the Professor of Anaesthesia, was unforgettable. Dr. Hattangdi's lectures in anaesthesia helped us enormously and he also shared our burden in looking after patients, sometimes relieving us of our daily chores. The two films I saw with Anjali, my wife, during the time was courtesy of Hattangadi. Before I proceed I must tell of my first day in the operation theatre block (MOT) in the consultants changing room, where I went on my own apprehensively, to discover its ambience. The only person there in OT dress was reading an Agatha Christie paperback with great seriousness. On entering he asked me as to who I was and then got up with great cordiality and shook me by the hands. That was Dr. Satish Nayyar, Assistant Professor in Surgery well known as he was a Hallet medalist in the primary FRCS examination. Dr. Satish Nayyar gave me a cup of tea and then said that I must cultivate some hobby (his was reading mystery novels) as Assistant Professors had nothing to do as the Professor usurped all the work which was worthwhile, while all the minor work was done by the Registrars (later called residents). I went into depression from which it took me a long time to come out. Within a week I took courage in my hands and went to talk it over with PNT. We decided that alternate cases would be operated by us while the other would assist. Matters went on well but I was perturbed over the fact that if he assisted, he would go out and talk to the patients attendants before I could come out. Again I went to him in 1968 and PNT graciously agreed he wouldn't do so. This was a remarkable thing at AIIMS. My struggle for identity of Assistant Professors went on to the faculty over such oligarchy and it was ultimately in 1970 that I was able to change the nomenclature of hospital units which hitherto were identified with the head, to that of the departments. Thus Prof. P.N.T's unit changed to Neurosurgery unit-a practice which continues today. I have always felt that to obtain the best from colleagues a measure of democracy and participation should be the prime substance PNT's contribution towards this was immense which allowed me to put my heart and soul in developing the department and later the Neurosciences Centre. I guess the role of wives is also very great. Our families (Tandon and Banerji) were close to each other and even today no major decision in the Banerji family takes place without Tandons consultation. I guess this meeting was lucky for both of us.
In 1969 Dr. S.K. Ghosh left for Goa on promotion as Professor and Neuroradiology was taken over by Dr. R.K. Goulatia for whom a separate post was created in neuroradiology. In mid 70's Dr. S.S. Saini was persuaded to join Neuroanaesthesia and this started the nucleus of a comprehensive clinical setup. Fortunately we were able to persuade (Mrs. D. Saini to join as our OT sister incharge and thus there was a feeling of family and belonging, so important in the development phases of any new venture. Dr. Subimal Roy was spending considerable time in Neuropathology to complete the picture. I had a vision of Neurosciences Centre akin to PNT, however I knew that basic neurosciences can never develop on its own because of economic compulsions. My emphasis was on developing clinical neurosciences and bring in basic neurosciences within its umbrella.
By mid 70's both neurosurgery and neurology had relocated itself on the main hospitals 4th floor and we were lucky to have separate independent wards. Mrs. M. Bindra joined us as sister I/C of neurosurgery ward and her dedication eventually made our ward the talking point of nursing care in the Institute. She eventually rose to become the Nursing Superintendent of the Neurosciences Centre.
In 1966 one day, walked into my office Dr. Brahm Prakash, who had resigned his Short Service Commission in the army and had married recently. He was at loose ends, asking my advise as to what he should do. He had earlier worked as my junior resident in general surgery at Medical College, Lucknow and the association was about 10 yrs. old. I persuaded him to join neurosurgery.We were able to rustle up the required formalities for starting MCh course with bare facilities but boundless enthusiasm. He was the first trainee and later joined our faculty and went on to become the Director Professor at G.B. Pant Hospital and started his own MCh programme. The AlIMS MCh course went from strength to strength and eventually we were having both the 5 yr and 3 yr streams. Neurology D.M. had started already in 1965. Now AlIMS trainees are spread all over India. Several headed departments e.g? Dr. Gourie Devi became Director Vice Chancellor of NIMHANS, Dr. B. Prakash at G.B. Pant Hospital Delhi, Dr. B.S. Das at NIMHANS, Dr. S. Mohanty at IMS, BHU Varanasi, Dr. A. K. Reddy at NIMS Hyderabad, and Dr. M.A. Wani at SKIMS Srinagar. Many hold important positions in teaching as well as private sector. We i.e. PNT and I are inordinately proud of all who trained themselves with us and wish them all the best in their future endeavors. Our wish is that they better us in their achievements. A major breakthrough in our clinical services occurred in 1976 with the coming of Prof. H.W. Pia who did a course in laboratory microsurgery. In the next few years we started a microsurgery laboratory and operative microsurgery was initiated. In the Indian scenario we stole the lead. In late 60's with the help of our ENT surgeon Dr. S.K. Kacker we started trans-sphenoidal pituitary surgery which consolidated in the 70's and became a routine procedure.
The process of development of the Neurosciences Centre in collaboration with the Cardiothoracic Sciences Centre started in real earnest in early 70's. Dr. N. Gopinath of Cardiothoracic Surgery and PNT were the architects. Land allocation was done by Prof. V. Ramalingaswami, the then Director AIIMS. Ghosh and Pradhan Associates were appointed architects and their started the planning for the basement, ground floor and the operation theatre block of our centre. Hours and hours of meetings with the architects-designing and tearing plans, it went on and on. I heard my wife say that I started talking of planning even in my sleep. We were about ready to have the foundation stone laying. This was 1977 and Mrs. Indira Gandhi's infamous emergency was coming to an end. One afternoon, in PNT's office, Dr. N. Gopinath suddenly said it would be nice to have Mrs. Gandhi lay the foundation stone. I had recently treated Mr. Dhawan's (then the personal secretary to Mrs. Indira Gandhi) nephew and I said shall I try. I rang him up on the phone from PNTs office. Mr. Dhawan immediately said yes and wanted probable days and times so that it could be confirmed taking into account Mrs. Gandhi's tour programmes. Elections were round the corner and Dr. Ramalingaswami wisely asked us to go slow. Mrs. Gandhi lost the elections and it is possible that the Janata Government which followed may have taken offence and delayed the start of the Centre had we got Mrs.lndira Gandhi to lay our foundation stone. Eventually, President Mr.Neelam Sanjeeva Reddy lay the foundation stone in 1978. When the building started many problems surfaced e.g. we suddenly discovered that there were very few toilets while most of the patients of cardiology were on diuretics and required use of toilets frequently. Again to the drawing boardbreaking of walls, laying of new sewer lines and so new toilets came into being. I know the OPD and of course the toilets have today become too inadequate with increasing number of patients coming to the Centre.
The brief period of Janata regime from 1977 and 1979 saw the irrepressible Mr. Raj Narain come as the Health Minister. All work in the Ministry came to a halt as also our Centre which bore the backlash of erratic ways of Mr. Raj Narain. The only thing I remember was meeting him near the present Community Medicine Department late in the evening,Mr. Raj Narain was coming to inaugurate, if I remember correctly, the Centre of Community Medicine. As usual he was hours late and the then Director Dr. L.P. Agarwal was standing with 3to4 faculty members. I tried slinking away but Dr. L.P. Agarwal called me and more or less forced me to stay on awaiting Mr. Raj Narain. He eventually came when the numbers of people waiting was not more than half a dozen. Before going to cut the ribbon he was introduced to all of us. He was highly intrigued with me and asked what would I find if I did have an opportunity to see the inside of the head of Mrs. Indira Gandhi. I made some polite comments though I was sure Mrs. Gandhi had a better quality brain than Mr. Raj Narain. Anyway he went on to narrate it with great gusto during a special convocation to award an Honorary D. Litt to Dr. Sewoosagar Ramgoolam of Mauritius. It was in such bad taste that Morarji Desai who was chairing frowned and all of us in the auditorium hung our head with embarrassment.
My two stints as Chief of Neurosciences Centre were significant in the development of the Centre. The first was a 2 year term as acting Chief of Centre while Dr. PNT was on Nehru Fellowship between 1984-86. This was the time when after the first phase of building (OPD, radiology wing, basement and OT block) we had reached a dead end as far as expansion of the Centre was concerned. Prof. M. L. Bhatia was the Chief of Cardiothoracie Sciences Centre. Our formal requests for funds were stiffly rebuffed by the then Joint Secretary Finance Adviser (JSFA) of Health Ministry. Ms. Sarla Grewal, widely nick named 'hunterwali' by her unkind colleagues, was the Secretary. We were advised not to try and influence her which could cause an unpredictable antagonism to our proposal. Anyway we went to meet her, placed before her, the developments till date, including our mounting clinical load, increasing public expectations, and the blockades experienced by us for expanding our Centres to what was originally planned. Ms. Grewal quietly listened to us, occasionally interjecting for a clarification. After we completed she asked for the JSFA who was the main stumbling block, to come and join the meeting. The moment he saw us his hackles were raised. On being asked by Ms.Grewal as to what were the problems in giving us the grant he started off with a long list of financial mismanagement by AlIMS in which our Centres had no role to play. (Most of the problems recounted were exaggerated to say the least). Ms. Grewal asked as to why our Centres were being penalised for what AlIMS had done. To this the JSFA said that this is a part of financial management for which he was responsible. Then we saw the legendary Ms. Sarla Grewal come into her elements. In chaste Punjabi she asked the JSFA as to who was the Secretary of the Ministry and how dare he speak to her like that. The poor JSFA spluttered and stuttered and tried to put in a word edgeways. Ms. Grewal asked him to leave the office and we knew that our battle was half won. However after leaving her office both Prof. M.L. Bhatia and I, as a matter of diplomacy, went to the JSFA's office. He was in the dumps. We nursed his hurt ego by asking for his help as we knew that he was quite capable of going to the Finance (Expenditure) Secretary and derail our proposals. I think the strategy worked as he did become a supporter. Of course things were helped as a few close relations of the JSFA fell conveniently ill at the same time requiring cardiac and neurosurgery. Funds eventually came though it took another year and in 1986 the remainder of the present Centre's building was started. Prof. P. Venugopal was a constant source of support in our endeavours. In the same period the next Union Health Secretary was Mr. Srinivasan, who was unenthusiastic about our Centres. His general impression was that we were overstaffed, our equipment underutilized and our clinical output low compared to other hospitals e.g. G. B. Pant Hospital Delhi, Christian Medical College Vellore, and certainly Apollo Hospital Madras which to him was the ultimate in financial management and output. Incidentally he was involved with the starting of Escorts Heart Institute which he clearly told us is a 'better bet than us'. Prof. Bhatia, Venugopal and I went through our records as well as what we could gather from the other institutions which Mr. Srinivasan thought had better quality and quantity of work. He had a meeting separately with our Neurosciences group to take stock. I had taken Dr. Baldev Singh and Dr. P.N. Tandon for the presentation made by me. By the end Mr. Srinivasan was convinced of the genuineness of our proposals. My plea at that time was to get financial grant equal to G.B. Pant Hospital whose output was half of ours. It was a landmark victory as our grants immediately increased, a trend which continued in the future.
My next stint as Chief of Centre was between 1988-95. Finances were forthcoming in good measure We had a CT scan and state of art angiography equipment. Our ICU was the best in the country. What we lacked was a MRI Scanner. I must pay special thanks to Mr. R.L. Mishra who was the Union Health Secretary in the latter part of my assignment. We had an excellent relationship and he was always positive in his approach. It is through his help that we got the NMR department setup at AIIMS, which was far more than merely obtaining MRI equipment. Incidentally even today the NMR Department has the only 2 Tesla machine capable of MR Scan and also MR Spectroscopy. The NMR department also has chemical NMR and the only experimental NMR in India today. It was an unique experience to create a whole department with the help of the then director Dr. S. K. Kacker who was always supportive.
It is during my tenure that proposals were sent to the Government for making the Centre the best equipped not only in India but in the Asian region. The Gamma Knife has started after I retired and I am sure PET scan and other newer equipment would come in due course.
I am often asked as to whether I have any regrets. My special regret is our offices being removed from the main Institute. It was originally envisaged that offices would remain where they were located i.e., adjacent to Anatomy dissection hall. The translocation has severed the umbilical cord to the other specialties in the Institute. This isolation does not augur well for the future of our Centre, as any branch of medicine to flourish requires interaction with sister disciplines. My other regret is the inability to have nonclinical neurosciences to come and establish themselves in our Centers new building. I had tried, even to the extent of keeping a floor vacant for one year under various pretexts.
My greatest gains were the colleagues I had - friends for life. I know I left alive vibrant active Centre which will only grow from strength to strength. Even today for anything I always say Neurosciences Centre, AIIMS is the best and with every breath only wish it the very best in its future endeavors.”

Prof.
P.N. Tandon
Others
Affiliation
Emeritus Professor
Department of
Neurosurgery
Contact
Email :
tandon@nbrc.ac.in
“The Departments of Neurology and Neurosurgery at the All India Institute of Medical Sciences were initiated in March 1965 with the appointment of Prof. Baldev Singh and myself as the first Professors. A neurology service in the Department of Medicine started by Dr. Jim Austin from the USA and later under care of Dr. Vimla Virmani was already in existence at that time. Significantly enough the Institute was, from its very inception, an important centre of neuroscience research. The first two Professors in Department of Physiology (Prof. B.K. Anand and Prof. A.S. Paintal) were undisputable leaders of neurophysiology in the country. Dr. Paintal had, however, already moved to Patel Chest Institute a year earlier, the remaining faculty members of the department were all pursuing neurophysiology research. Prof. Keswani, the Chief of Anatomy, was primarily interested in neuroanatomy. Prof. G. P. Talwar, at that stage, was enthusiastically involved in researches in neurochemistry This was of course before his shift to immunology. Acknowledging these strengths International Brain Research Organization (IBRO) had already held one of its earlier workshops in the Institute. Dr. Sriramachari, Deputy Director of Indian Council of Medical Research, though not on the faculty of the Institute freely provided his services for all neuropathological work till several years later when Dr. Subimal Roy took over the responsibility fully. While clinical neurology and neurosurgery departments existed at several centers in the country much earlier; even the oldest such centers at Vellore, Madras, Bombay and Calcutta, did not have such broad base of neuroscience as we were fortunate to have at the Institute. Given the overall milieu of rapid growth and development in the institute at that time, the clinical departments also expanded rapidly. It will be hard for the current staff and students of the Institute to visualize how close interaction existed among all these departments and units in the earlier years. This was in no small measure due to the all pervading influence of Prof. Baldev Singh real father figure for all of us.
The idea of establishing a "Brain Research Centre" at the Institute had already been envisaged by Prof. B.K. Anand even before the clinical departments came into existence. No doubt this was primarily thought of as a basic research centre. Thus on 1st December 1964, Dr. Anand vide his letter No. Phy/64/1235 requested the Director for initiating steps for developing a Brain Research Centre" with the existing ICMR Neurophysiology unit as its nucleus. Unfortunately no action was taken on his request.
In 1968, when the Institute was to formulate its development plans for the Fourth Five Year plan of the Government, Prof. Anand, Prof. Baldev Singh and I had several informal discussions to once again revive the proposal for a Brain Research Centre. It may be mentioned that, not surprisingly, this proposal was heavily loaded in favour of creating research laboratories including a couple for neurology and neurosurgery. While we were heavily constrained in our clinical work due to limited diagnostic and operative facilities at this time we went along with Prof. Anand in supporting this proposal hoping to strengthen the patient care services through the development plan for the Institute hospital which was to be commissioned
The Development Committee approved the proposal in principle, but owing to financial constraints no concrete steps were taken. The Institute Body ultimately agreed to create a few staff positions so that "Centre can make a start as early as the Financial Year 1970/71. In practical terms it amounted to absorbing some of the staff of the Indian Council of Medical Research Neurophysiology Unit and nothing more.
When we finally shifted to the new hospital the Neurosurgery Department had 22 beds allotted to it. We had one operation theatre, but no specialized neurosurgical operation table and no intensive care unit. The neuroradiology set up consisted of a skull table without automatic changer for angiography, no facilities for tomography nor a dedicated unit for myelography. Isotope encephalometry then a routine diagnostic investigation abroad was nonexistent. We had an EEG machine but no facilities for EMG or nerve conduction. Nonetheless we were facing increasing demands for patient care from all over the country and also our neighboring countries. Waiting lists for admission and surgery were a constant source of worry for us and frustration for the suffering patients. We had already started the M. Ch. course.
Similar problems were being faced by the Cardiology and Cardiothoracic Surgery Departments. One day in 1971 when Prof. Gopinath and I were scrubbing for surgery in the common scrub room between our two theatres, he informed me that they have submitted a proposal for a Cardiothoracic Centre "Why don't you also do so, otherwise we will never progress". I, therefore, once again took up this matter with Prof. Anand who was now also the Dean and sounded the Director, Prof. V. Ramalingaswami. On receiving a favorable response, it was decided that, unlike in the past, our proposal this time should be a comprehensive one, including parallel development of basic neurosciences and clinical disciplines. Dr. Manchanda along with Prof. Anand formulated the proposal in respect to basic neurosciences. I, in consultation with Prof. Sumedha Pathak, the then Professor and Head of Department of Neurology and on the advice of Prof. Baldev Singh and Dr. Banerji prepared the plan for the clinical centre. A draft proposal was thus submitted on 16`" July 1971 to the Dean with the comments "in view of the present extent of development at the Institute to start with emphasis will be on neurophysiology, neurology and neurosurgery. Nucleus for the following will be established with a view to development of these into fully fledged specialties, as integral part of the centre, as personnel and fiscal resources were available". These included neuroanatomy, neurochemistry, neuropathology. This proposal was discussed by Prof. Baldev Singh (who was now an Emeritus Professor) with Prof. B.K. Anand who agreed with it fully and desired to "go ahead and fill up all the details regarding space, equipment, personnel etc. working out the cost" etc. We agreed to change the name from Brain Research Centre to Neurosciences Centre. We had a detailed and somewhat ambitious plan formulated. Though the plans were ready there was no obvious source for funding it. Was it going to be another document for the archives? This thought remained a constant worry, Prof. Ramalingaswami was fully in agreement but was finding it difficult to find funds for it.
Several months passed. One day while casually discussing our mounting frustrations with lack of any progress with my elder brother, who was then a Jt. Secretary in the Prime Minister's office, I initially got a cautious reply, "Prakash, officially I do not wish to get involved in any thing that may be considered as a favour to my brother. The only thing I can do is to arrange a meeting for you with the PS to the Hon'ble Minister of Health Shri Uma Shanker Dixit. Even before that, first take the permission from your Director to do so". It was easy to obtain Director's permission and shortly afterwards a meeting was held with Shri Rajgopal, who was more than sympathetic to our request for establishing the Neurosciences Centre. At the end of the meeting he told me that it was not possible to get such a major scheme funded in the middle of a plan period but "may be we could get advanced action initiated which can then be formalized in the next plan". He promised to discuss this with Dixitji at an appropriate time. The meeting ended with encouraging but cautious note, "I promise nothing but I am convinced it is a genuine need. You are asking nothing for yourself? you are willing to provide more and better service to those knocking at your door".
Not expecting any prompt action I was pleasantly surprised to receive a call from the Director later that evening, "Health Secretary Shri K.K. Dass wants us to include the matter related to the establishment of the Neurosciences Centre in the agenda for the next meeting of the Institute Body due shortly. He wants a copy of the proposal sent to him in advance". On 2nd August 1972, a copy of the formal proposal was duly sent to the Shri K.K. Dass by the Director. At the Institute Body meeting held on 12'" September 1972, the Institute decided, "The Institute considered that it was fortunate that expertise in several fields of Neurosciences exists at the institute both in basic and clinical areas. The Institute considered the scheme put up for its consideration as possible, desirable and in the larger interests of the country. Recognizing the strengths already built in the various departments in respect of the neurosciences, the Institute approved the proposal in principle to set up a Centre for Neurological Sciences at the AIIMS and decided that not only it be included in the proposals for the Fifth Five year Plan of the AIIMS but, the possibility of advance action in the Fourth Five Year Plan itself, should also be seriously explored. It was accordingly decided that the matter be considered by the Finance Committee in greater detail". We felt happy but not jubilant, fully conscious of the harder battles ahead
The Proposal was duly put up to the Finance Committee meetings held on 4th January 1973, 8th February 1973 and 5th April 1973 and as feared owing to "financial constraints" no funds could be made available. The real reason was no doubt that Shri K.K. Dass had retired by now and his successor Shri Ramachandran had his own antipathies against the Institute as future events confirmed.
However, without waiting for a formal decision of the Finance Committee, Prof. Ramalingaswami forwarded the proposal to Dr. Banwari Lall, Chief, Health Division, Planning Commission for his consideration. Dr. Lail was a close friend of Prof. Anand who arranged a meeting with him in the Planning Commission after Dr. Lall had opportunity to scrutinize the proposal. With high hopes Prof. Anand and I attended the meeting. To our surprise Dr. Lall, after a brief discussion, said, "Bal (B.K. Anand), I am sorry this proposal as it stands is unlikely to be approved owing to severe financial constraints. The only component that may be favorably looked at is the patient care part". He also made several suggestions for curtailing the budgetary demands even for the clinical component. It was with a sense of disappointment that we walked out of his office. I was, in addition assailed with the fear of losing Prof. Anand's interest and support for the project. Probably sensing my thoughts, on our way to the exit he suddenly stopped said, "Prakash, it is too bad to have things take a turn this way, but let us be practical. We should take whatever we can get and keep trying for the rest. You will have my full support". Few in his place could have been so generous and even more so the enthusiastic support we continued to get from him later on provided enough proof of the genuineness of these sentiments. For all this he no doubt, got the flak of his colleagues in the Physiology Department.
In pursuance of the decision of the Institute Body and the informal advice received from Dr. Lall we carried out another detailed exercise to draft a formal EFC (Expenditure Finance Committee) memo. In the meanwhile Prof. Gopinath had carried out a similar exercise for the Cardio-thoracic Centre. As a matter of fact, these exercises were mostly done with the constant consultations with each other. Combined these two proposals required considerable financial support. Dr. Ramalingaswami advised us that we should seek the views of the new Health Minister Shri Khadilkar. After a patient hearing of our individual proposals, he pointed out the difficult financial situation and advised that we should try and economize by establishing some common facilities and sharing whatever can be shared thus bringing down the total cost of two proposals. He promised to get the demands included in the Fifth Five Year Plan proposals of the Institute. Thus Prof. Gopinath and I carried out another exercise maintaining the basic character of two independent centers, yet having some common areas and support laboratories. On 2nd August 1973, a new draft proposal was forwarded to the Director with a note, "In view of the difficult economics situation, we (Profs. Anand, Gopinath and Tandon) have also reviewed the projects with an idea to prune these without undue detriment to the utility of the projects". And further, "Following this review, if we could get a total of Rs. 350 lakhs (Rs. 200 lakhs for Cardiothoracic and Rs. 150 lacs for Neurosciences Centre), we could still make a worthwhile contribution".
The Planning Commission, discussed the proposals of the Health Ministry (which included those of AIIMS) on 31st August 1973. The bias of the Health Secretary, Shri Ramachandran against the institute was too obvious. He had proposed a total of Rs. 150 lakhs for the whole Institute. As a matter of fact it was specially emphasized that the Ministry "did not favor that all the specialties should be concentrated in one place in the country". Following strong pleadings by the Director, one of the members of the Planning Commission, Member (M), pointed out that "the Ministry had proposed Rs. 1.50 crores for the AlIMS as against the Fourth Plan provision of Rs. 3.33 crores, and since this was a premier Institute in the country, the Ministry may explore the possibility of providing some additional funds for the Fifth Five Year Plan. With regards to the proposals for the two centers, the Planning Commission ultimately decided to allocate separate funds for "the development of super-specialties: a total of 236 lakhs, without specifically mentioning our proposals. This was a typical bureaucratic stroke by the Health Secretary to scuttle our proposal. Before implementing the program, the Ministry of Health decided to enquire from all medical institutions in the country to submit their proposals for "development of super-specialties", notwithstanding the fact that the Central Government is supposed to directly fund only the national institutes. As expected proposals were received from several places and interestingly even Orthopaedics was considered a super-specialty. The Health Ministry, obviously under the instructions from its Secretary put the whole matter in the cold storage with the usual excuse, "the matter is under consideration": even though the Fifth Plan had already begun from April 1974.
One day Dr. Karan Singh, who was now the Minister of Health, desired to see me for some unconnected reason. At the end of our meeting, I enquired about our proposals for the centers. Only then the cat came out of the bag. He frankly informed me that the Secretary was sitting on the file on the excuse of collecting information mentioned above. Dr. Karan Singh recognized the futility of the exercise. Since in the limited funds allocated for super specialities it would be impossible to meet the needs of even a few. He promptly took the initiative and in August 1974 appointed a committee under the Chairmanship of Dr. Srivastava, the Director General Health Services, to assess the existing potentials and future possibilities of strengthening superspecialities in the centrally funded institutions only. The Committee included experts in the concerned disciplines from all over the country. It collected the necessary information from various institutions and finally paid site-visits to each of these before recommending our two proposals alongwith some allocations to a couple of others. Thus from a total of Rs. 236 lacs allocation for super specialities the two Centres at the AIIMS, was provided Rs. 188.37 lacs.
On March 26, 1975, even before we received a formal approval of the Government to establish the Centre, a letter addressed to the Director, AlIMS received from Dr. Sharad Kumar, DDG(M), indicating that, "Under the Purely Central Scheme of "Development of Superspecialities', the Government of India has sanctioned a provision of Rs. 10 lakhs for the development of the Departments of (1) Neurosurgery and Neurology; and (2) Cardiology and Cardiothoracic Surgery...............”
This communication, though not mentioning anything about the Centers, was the first indication that the Government had selected AIIMS; for development of these super-specialties. Two weeks later on 11th April 1975, the recommendations of the "Expert Committee on Establishment of Cardiothoracic and Neurosciences Centre at the Institute", were ultimately received, setting at rest all uncertainties about the two proposals. It would be worth reproducing the extracts of this communication with respect to Neurosciences Centre (see Dr. Sharad Kumar's letter dated 11th April 1975). Shortly afterwards on 22"d July 1975 a formal letter from the Ministry of Health and F.W. No. V. 16020/54/ME (PG), communicated to the Institute an allocation of Rs. 188.37 lacs for the super-specialties (including both centers) for the 5th Five Year Plan. It needs to be recorded that the fullest understanding between Prof. Gopinath and myself and the cooperation of the rest of the faculty of the concerned departments made it possible for us to keep on revising and redrafting the proposals as per the bureaucratic needs of the Government, without sacrificing the basic objectives. No hidden rivalries, personal egos or unjustified interests of individuals ever cast any shadow as we pursued the planning and implementation of the projects through various administrative channels. For me it was a rare experience of trust and camaraderie not so common in our institutions.
As expected it was not smooth sailing from now onwards. We had to wait till March 1976 for the first release of funds, a paltry sum of Rs. 3 lacs. At one stage the Financial Advisor to Ministry of Health, whose main grudge against the Institute happened to be "misuse of funds for erecting black marble columns in the foyer" without any justification reduced the total allocation for the Fifth Plan by nearly Rs. 40 lacs, probably worrying that we would waste it on black marble columns. When no explanation and assurances from Dr. Gopinath and myself failed to convince him, we had to approach the office of the Finance Minister (Shri C. Subrramanayam) and the Planning Commission Deputy Chairman Shri P.N. Haksar, two of the most progressive policy makers of the country has known. Let me hasten to add that Prof. Gopinath and I approached them with the approval of our Director.
In July 1976, the Estate Committee formally appointed M/s. Pradhan Ghosh and Associates as the architects. However, between 1976 and 1978 repeated revisions of the building plan were required due to pruning of the budget allocations and rising cost of the building. At last on 14th April 1978, the President of India Shri Neelam Sanjiva Reddy laid the foundation stone of the twin centers. In his welcome address Dr. Ramalingaswami stated, "Our vision of the Centers is that they will be Centers both of public service and of higher learning at the same time". Their philosophy is that in which the patients and their needs come first, everything else is subordinate and subservient to this: He pointed out that, "The greatest and deepest need of a Centre is to be needed by Society". Quoting the famous economist Francis Delaisi, he said that. "the purpose of an Institution is to supply stability needed for long term operations. At the same time, Institutions must be able to adjust to change. It is our hope that stability, adjustability and continuity will mix in the centers in appropriate balance". Rashtrapatiji in his address expressed his happiness on the establishment of these Centers. While emphasizing that, "Our most urgent need is Primary Health Care" which should be pursued with all energy and resources at our command." He pointed out that, "we cannot altogether neglect the setting up and improvement of more advanced levels of health care at District, State and national levels. We need to have a few Centers of excellence in a large country like ours where the most advanced levels of care can be provided; specialists and researchers can be trained and the most complex problems may be referred for appropriate management" For him, "It is not a question of this or that" but a "proper balance in the developments of these various levels of health care". He was equally concerned about the scientific community which must be able to discover, adopt and innovate suitable methods not only in dealing with our current problems but also in coping with changing trends and changing needs of the future". I have quoted these excerpts from the speeches because I believe that as long as we pursue these ideals the Centre would continue to justify the generous resources provided by the government and enjoy the trust of the people.
Five years later, in March 1983, out patient clinics for Neurology, Neurosurgery (as also Cardiology and Cardiothoracic Surgery) moved to the new building, while the work continued to complete the rest. Progressively as the work progressed we continued to occupy the areas already completed. By July 1984, the built up area included basement, OPD, receiving station, noninvasive laboratories, radiology wing, 8 operation theatres (Neuro 3, Cardiac 4, Common 1) along with ICUs and postoperative wards. It was only in 1988-89 that the Centres became fully functional in their new abode. At this time Neurosciences centre had a total of 180 beds, 3 fully equipped operation theatres, 30 bedded ICUs, Intermediate care wards, fully fledged departments of Neuroradiology, Neuroanaesthesia, within this complex. The offices of the faculty and supportive staff, Neurochemistry laboratories continued to remain in the old building and by mutual agreement the Neuropathology still continues to be in parent Department of Pathology. This may be compared to the facilities available to us before we moved to the Centre. The combined strength of beds for Neurology and Neurosurgery including a half baked ICU was only 72, scattered in different parts of the old hospital.
There was only one dedicated operation theatre for neurosurgery and we shared another one with Cardiothoracic Department three days a week. There were four members on the faculty of Neurosurgery. I have been informed that there will be separate write-up's about the development of Neurology, Neuroradiology, Neuroanaesthesia, Neuropathology, Neurochemistry etc. hence I shall restrict myself in the remaining part of this review on Neurosurgery only. Nonetheless it should be mentioned that once the scheme for creating the Centre was approved, in the interval before its complete occupation we were permitted to augment the overall facilities and staff strength in a progressive manner with a view to improve the quality and maximise output of all our activities-patient care service and education in particular. Funds for research had, as even now, to be obtained on competitive basis from the grant giving agencies. During this interval we were able to obtain a munificent grant from the Swedish International Development Agency (SIDA) which modernized our diagnostic and clinical facilities including those for operation theatres and ICU. The first CT Scan in the country was installed under this grant. It was not just a coincidence that this was inaugurated by the President of India on the same day as the foundation of the Centre(s) was laid.
Coming back to the growth of neurosurgical services, in the first full year of our work i.e. 1966 we admitted 140 patients, attended to 540 in the OPD and performed 111 major and 89 minor surgical procedures. It may be mentioned that at that time many of our patients were admitted, operated upon and discharged from the emergency ward. Five years later in 1971 these numbers were 422 admitted, 1044 attended in OPD and 535 303 major and 232 minor operations performed. In 1976, the year when the first token grant was received for the Centre we admitted 1094 patients, attended to 3784 (1960 new and 1824 old) patients in the OPD, and performed 520 major and 785 minor surgical operations. It may be recalled that at that time neuroradiological investigations pneumoencephalography ventriculography, angiography and myelography were performed by. the clinical team and hence were included as minor operations. In 1986, prior to shifting to the Centre 1898 patients were admitted, 11.225 (3406 new and 7918 old) patients seen in the OPD and 735 and 257 major or minor operations were performed. Starting with only two faculty members in 1965 - Dr. Banerji and myself, it was only in 1971 that we added one more lecturer. Dr B. Prakash. The next person to join was Dr R. Bhatia as Lecturer in 1974 The first faculty position in the Department of Neurosurgery after the Centre came into existence, was 1979 with Dr. Banerji taking over as a Professor. A little known episode in this connection needs mention to illustrate the prevailing team spirit at that time. When we got the first position of a Professor sanctioned for the Centre, I had in my mind wanted it for Dr. Banerji. The day the matter was to be finalized in the Academic Committee I was indisposed and requested Dr. Banerji to attend the meeting and briefed him about my plan. His immediate response was that it should be alloted to Neuropathology, "Dr. Subimal Roy should be given a chance before me". Dr. V.S. Mehta then joined as a Lecturer in 1981 followed by Dr. A.K. Mahapatra in 1983. In the meanwhile Dr. B. Prakash left for G.B. Pant Hospital in 1980. Thus even after fully commissioning the Centre in 1988, the Department had a total strength of 5 faculty members; who continued to share the ever increasing service load as indicated by the figures provided above.
Education
Besides the full fledged in-service M.Ch. course (3 years for post MS (surgery) and a direct 5+1 year after MBBS), the department has been participating in undergraduate education as well as collaborating with basic science department for Ph.D. program. From 1968 when our first trainee obtained his M.Ch. degree, till 1988, twenty eight persons obtained their postgraduate degrees. Since 1988 up to date an additional 31 have qualified. Most of these are serving the country. Several of them became chiefs of their departments at Delhi, Varanasi, Srinagar, Bangalore, Cuttack and Hyderabad, thus fulfilling an important objective for which the Centre was created. From its inception the Department has been actively engaged in CME programs both intramural and extramural. Short-term training programs are organized regularly on recent advances like CT scanning, Microsurgery, Neural Transplantation, Vascular Surgery, Skull base surgery etc. An yearly course on Neurobiology for Clinicians was organized (4 at the AIIMS and 1 at NIMHANS, Bangalore). National level Hands-on Workshops were organized from time to time with the help of international faculty as for example on microneurosurgery, skull-base surgery, neural transplantation etc. A microneurosurgical laboratory, the first of its kind in the country, was established for training in microsurgical techniques, not only for neurosurgeons but for others specialities also from all over the country. The first National Neural Transplantation Facility was established in collaboration with the Department of Anatomy. The first Text Book of Neurosurgery in the country was the result of a joint effort between Madras Neurological Institute and AlIMS in 1980. This has been completely revised and updated in 1996. Four monographs "Lectures in neurobiology" were brought out in collaboration with the Department of Anatomy, AIIMS. The faculty has made contributions to several national and international text books including Tropical Neurology, Handbook of Neurology and Techniques in Neurosurgery.
Neurology and Neurosurgery Centre cont.
The Committee has further observed that
- Minimum arrangements have to be made to coordinate the emergency and head injury service of the Safdarjung Hospital with the Neuro-centre by:
- according mutual and appropriate designations for the staff of each institution in the other; and
- arranging full clinical coverage of these beds by the combined staff of the Neuro-Centre and delineating mutual responsibilities.
- The Neuro-radiological facilities already available in the Safdarjung Hospital, including one Mimer X-ray machine, must be made available for this Neuro-Centre immediately, alongwith early sanction of the recommended neuro radiology staff.
- Experienced Neuro-pathologists being very few in the country, the Committee strongly recommends the immediate appointment of Dr. S. Sriramachari, Director, Registry of Pathology, New Delhi, as the Hony. Professor of Neuro pathology in this Neuro-centre
- The various sub-sections collaborating from the parent departments in the AlIMS should. in course of time, become full-fledged departments of the sub-speciality - e.g. neuro-pathology, neuro-radiology, neuro-physiology, neuro-chemistry, neuro-psychology etc.”
Research
AlIMS provided a unique milieu for advancing frontiers of knowledge. The Neurosurgery Department fully participated in this effort The major areas of research contributions of the Department involved collaboration of other departments in the Institute and outside included;
- Head Injury: epidemiology, intracranial hematomas and temporal lobe lesions, brainstem injuries, growing skull factures, outcome of severe head injury. Those studies included a collaborative investigation with Institute of Neurology, Madras and another with University of Charllotesville, Virginia, USA. With in the Institute departments of ENT, Ophthalmology, Pathology, Radiology and Medical Jurisprudence were parts of the investigations at various stages.
- CNS Tuberculosis experimental studies on pathogenesis, clinical manifestations, etiology and management of post meningitic sequelae, neuroimaging. evaluation of therapeutic modalities (These studies were carried out in collaboration with the Departments of Microbiology, Pathology and Radiology and Nuclear Medicine).
- Brain Abscesses: Etiopathology, clinical manifestations, brain abscess in cyanotic heart disease, subdural abscesses, management strategies.
- Cysticercosis: its clinical manifestations, diagnostic dilemmas, CT imaging, role of surgery.
- Brachial Plexus injuries: a series of investigations as one of the largest in the world, included problems of diagnosis, evaluation of surgical procedures. These studies have been carried out in collaboration with Department of Neurology.
- Optic nerve injuries are a subject of prospective investigations for more than a decade. Clinical manifestations, visual evoked potentials, role of surgery have been evaluated in collaboration with the department of ENT and as a part of an international multicentric study.
- Subarachnoid hemorrhage and Intracranial aneurysms specially epidemiological, etiopathological investigations and studies to evaluate various management strategies. The initiation of these studies was done as a part of a multicentric national study which proved the fallacy of the prevailing view of rarity of intracranial aneurysms in India
- Pituitary Tumours: Immunohistochemical classification, correlation of clinical-pathological and hormonal profile, tissue culture studies (These studies were carried out in collaboration with the Departments of Endocrinology and Neuropathology). Most of these studies were initiated after Trans sphenoid surgery had been established, for the first time in India, in collaboration with ENT department.
- Gliomas: were a subject of a series of investigations on pathology, classification, evaluation of growth potentials, prognostic factors etc. Surgery for gliomas of the dominant hemisphere constituted a major thrust. A large number of investigations including EM, immunohistochemistry, in-vivo and in in-vitro labeling index studies, tissue culture and molecular markers have been carried out by the neuropathology department.
- Experimental studies on intracranial hypertension elaborated the patho-physiological mechanisms based on a biomechanical model. These studies were carried out in collaboration with the Department of Physiology at AlIMS and Biomedical Engineering at Indian Institute of Technology, Delhi. In another series of investigations with the Department of Pharmacology the pathogenetic mechanism of pulmonary oedema in raised ICP was elaborated.
- Experimental neural Transplantation: A national fetal Neural Transplantation Unit (supported by Department of Science and technology) was established in collaboration with the Department of Anatomy. A number of original contributions were made through a series of papers.
The above account will testify that much has been accomplished, no doubt a lot more needs to be. For me personally it has been a rewarding experience and source of great satisfaction, not just the physical growth of the Centre but the years of affection and friendship of the team who really made this happen. The only regret that continues to haunt me is our failure to see a parallel growth of the basic neurosciences as an integral part of the Neurosciences Centre. Individually these disciplines in the Institute have made very outstanding contributions. It has been stated that an institution is the lengthened shadow of an individual. If there is one example to disprove this adage, the Neurosciences Centre is one. It was born in the dreams of several, nurtured with the selfless, dedicated services of many who submerged their egoes for a cause greater than themselves, working as a team the parallel of which could hardly be found any where. In the true spirit of Gita, their sole concern was duty and not the reward. No sacrifice was great enough for establishing a centre of excellence. Posterity will judge whether they succeeded on not but no one would deny that they attempted. Unlike many other such centres in our country, even after the departure of those who initiated it, the Centre continues its journey to greater heights as will be obvious from the story told by those who succeeded. I hope and pray that the Centre will continue to live up to the foundation stone. "In the ultimate analysis, it is not the budget, nor the number of staff positions that makes a truly great centre of public service and higher learning. It is the presence of thoughtful, imaginative, humanistic, loyal and devoted faculty and students that is vital". The Centre continues to be endowed with them and I can only wish them greater heights in years ahead.
Recommendations of The Committee on Establishment of Neurology and Neurosurgery Centre at the AIIMS and Safdarjang Complex
This Centre has been chosen for the following reasons :
- The excellent staff that are in position and the very good record of patient care, teaching and research, particularly at the AlIMS.
- The existence of the supporting departments of basic sciences which are fully equipped and which can provide initially the nucleus for each ancillary department of the proposed Neurosciences Centre.
- The proximity of the department of Neurology at the Safdarjang Hospital which can serve as a trauma and emergency unit for this proposed centre.
The needs of this proposed Neuro-centre are indicated in Appendix I and may be seen to be economical and the minimum required.
This recommendation to make the neurology complex of the AlIMS and Safdarjang Hospital into a Neuro Centre is based on the following requirements.
- Enthusiastic cooperation from the Departments of Anatomy, Physiology, Biochemistry, Pathology, Microbiology, Endocrinology, Genetics, Immunology and Experimental Medicine and Surgery of the AlIMS and their capacity to provide the necessary staff and equipment to develop these special aspects like neuro-anatomy, neuro-physiology, neuro-pathology, neuro-chemistry etc. that is, a pooling of the resources already available. As this Neuro-centre develops and the national resources improve, each one of these sub-specialities may develop its section in a new building to be constructed.
- Expansion of the bed strength facilities will need space not available in the present building. A piece of land has already been earmarked to build a Neurocentre which has to be taken up on a priority basis.
- Till such times as the building is ready, the rest of the recommendations may be given effect to immediately.

Dr.
Shashank Sharad Kale
Male
Affiliation
Department of
Neurosurgery
Contact
Email :
skale67@yahoo.com
Phone :
26594888
General OPD
Tuesday - 9 AM to 12 AM
Saturday - 9 AM to 12 AM
Saturday - 9 AM to 12 AM
Brief Profile:
Striving to provide comprehensive spine care at the Neurosurgery Department AIIMS by dealing with complex cervical, occipito-cervical, thoracic, lumbar and sacral pathologies, tumors, and fusion and fixation, operations has been a constant endeavor. The department is now fully equipped to deal with complex spinal problems with the latest technological advances including Image guided workstation. The minimal access system for spinal surgery is being procured. A research laboratory with facility for cadaver dissection and spinal operations on experimental animals with drill, microscope and computer aids is under development has been developed.
My special area of interest is the cranio-vertebral junction. I have documented one of the largest series of patients in the world on developmental CVJunction anomalies and their management- almost 800 patients. Research on TB of the CV Junction – experience of 75 patients is under consideration for publication. Research of spinal TB with severe neurological deficits in 45 patients has been accepted for publication in Journal of Neurosurgery Spine. In the last 3years I have been invited to lecture/chair sessions/seminars on spine surgery topics all over the country and in international meetings. I have been nominated the Course Chairman for the AOSpine courses at Davos Switzerland attended by more than 300 spine surgeons from 80 countries in the world.
Inpatients: NS2 ward
Operation Theatre: NSOT First Floor CN Centre
Unit: Neurosurgery Unit II
Number of Beds: 47 + Private Wards
Intra-tumoral drug delivery for anaplastic astrocytoma trial; Cervical spondylotic myelopathy
- Have cranio-vertebral junction anomalies been overlooked as a cause of vertebro-basilar insufficiency? Agrawal D, Gowda NK, Bal CS, Kale SS, Mahapatra AK. Spine. 2006 Apr 1; 31(7): 846-50.
- Trans-cranial Doppler in severe head injury: evaluation of pattern of changes in cerebral blood flow velocity and its impact on outcome. Ojha BK, Jha DK, Kale SS, Mehta VS. Surg Neurul. 2005 Aug; 64(2): 174-9; discussion 179.
- The role of somatosensory evoked potentials in spinal dysraphism – do they have a prognostic significance? SSKale, AKMahapatra. Child’s Nerv Syst (1998) 14:328-332.
- Effect of whole-body vibration on the low back – A study of tractor-driving farmers in North India A Kumar, MVerghese, PMahajan, PGulati, SSKale. SPINE 1999 Dec 1; 24(23): 2506-15.
- Effect of whole-body vibration on the low back – A study of tractor-driving farmers in North India. A Kumar, MVerghese, PMahajan, PGulati,SSKale. Selected for Publication in the YEAR_BOOK of Orthopedics, 2000.
- Effect of whole-body vibration on the low back – A study of tractor-driving farmers in North India. A Kumar, MVerghese, PMahajan, PGulati, SSKale. Selected for Publication in the YEAR_BOOK of Orthopedics, 2000.
- Partial aplasia of posterior arch of the atlas with isolated posterior arch remnant: findings in 3 cases. A Sharma, SBGaekwad, PSDeol, NKMishra, SSKale. American Journal of NR Jan 2000 Jun-Jul; 21(6): 1167-71.
- Current Anterior Techniques for Single-level Cervical Disc Diseases Kale, DWCahill. Contemporary Neurosurgery. 2002 April.
- Isolated central canal rupture of spinal dermoid: report of two cases. AGarg, SBGaekwad, VGupta, NKMishra, SSKale. Australasian Radiology. 2003Jun; 47(2): 194-7.
- Craniovertebral junction abnormalities with vertebrobasilar ischemia. Gaekwad SB, Gupta V, K Avinash, Garg A, Suri A, Kale SS, Mishra NK. Accepted for publication in Special issue of the “Revista di Neuroradiologia” in 2003.
- Same as above: on the website of the Symposium: Symposium neuroradiologicum.org.
- Bipartite atlas with os odontoideum: case report. Garg A, Gaikwad SB, Gupta V, Mishra NK, Kale SS, Singh J. SPINE. 2004 Jan 15; 29(2): E35-8.
- Evaluation of Tc99m-glucoheptonate for SPECT functional imaging of medulloblastoma. Barai S, Bandopadhayaya GP, Julka PK, Kale SS, Kumar R, Malhotra A, Haloi AK, Seith A, Naik KK, Dhanapathi H. J Clin Neurosci. 2005 Jan; 12(1): 36-8.
- Evaluation of 99mTc-L-methionine brain SPECT for detection of recurrent brain tumor: a pilot study with radiological and pathological correlation. Barai S, Bandopadhayaya GP, Julka PK, Kale SS, Malhotra A, Haloi AK, Seith A, Gopendro Sing N. Acta Radiol. 2004 Oct; 45(6): 649-57.
- Intracranial gliofibroma mimicking a meningioma: a case report and review of literature. Deb P, Sarkar C, Garg A, Singh VP, Kale SS, Sharma MC Clin Neurol Neurosurg. 2006 Feb; 108(2): 178-86.
Original Articles National Journal
- Multifocal intracranial rhabdoid tumor. Suri A, Singh VP, Kale SS, Mehta VS, Gaikwad S. Neurulogy India 2003 Jun; 51(2): 297-8.
Chapters in Books
- Complications of Posterior Fusion Operations – S Kale, R Patir. C V Junction Anomalies- an Indian Experience. Ed: Dr. V K Jain, S G P G I Lucknow India 1997.
- Pterional Approach for Sellar and Parasellar Tumours – S S Kale, V S Mehta in Textbook of Operative Neurosurgery. Ed: K Sridhar, R Ramamurthy. (In press)
- Microsneurosurgery of craniopharyngiomas – S S Kale, V S Mehta in Proceedings of Microneurosurgery workshop conducted at A L S Neurosurgical Centre, V H S Medical Centre, Madras India 1998.
- Acute trauma and post-traumatic deformity of the occipitocervical junction.SS Kale, D W Cahill. Textbook of Neurosurgery. Ed: D W Cahill. In Press.
- Cervical Spine fusion in Rheumatoid arthritis. SS Kale, D W Cahill. Textbook of Neurosurgery. Ed: DWCahill. In Press.
Abstracts
- Developmental Osseous craniovertebral junction anomalies: Dilemmas and Controversies. Suri A, Kale SS, Chandra PS, Chabra MS, Mahapatra AK, Mehta VS. Neurosurgery Vol 51(2) August 2002.
- Cranio-vertebral junction anomalies with vertebro-basilar ischemia. SBGaekwad, VGupta, AGarg, GVRamdas, SSKale, NKMishra. Journal of Neuroradiology Aug 2002.
- Pre-op and Post-op SSEP in Spinal Dysraphism – an initial report. SSKale, AKMahapatra. Neurology India (Suppl) vol 42 1994.
- Complications of Posterior Fusion Operations – SSKale RPatir. Neurology India (Suppl) vol 45.1997.
- Spinal Dural A V Fistulas – an AIIMS Experience. AVarma, VSMehta, RPatir, SSKale. Neurology India (Suppl) vol 45 1997.
- Atlanto-Axial Complex Injuries – an AIIMS Experience. SSKale, BKOjha, AVarma, AJindal. Neurology India (Suppl) vol 47 1999.
- Role of Transcranial Doppler in the follow-up of direct carotico-cavernous fistulas undergoing balloon embolization. TArora, VSMehta, NKMishra, SSKale. Neurology India (Suppl) vol47.1999.
- Role of micro vascular Doppler in. Intracranial Aneurysm Surgery. PKumar, VSMehta, SSKale, VPSingh. Neurology India (Suppl) vol47.1999
- Transcranial Doppler ultrasound in severe Head injury. BKOjha, VSMehta, SSKale. Neurology India (Suppl) vol 47.1999.
- Hyponatremia in spontaneous subarachnoid hemorrhage. PKumar, SKale, VSMehta, SVaishya. Neurology India (Suppl) Vol 47.1999.
- Have cranio-vertebral junction anomalies been overlooked as a cause of vertebro-basilar insufficiency? Agrawal D, Gowda NK, Bal CS, Kale SS, Mahapatra AK. Spine. 2006 Apr 1; 31(7): 846-50.
- Trans-cranial Doppler in severe head injury: evaluation of pattern of changes in cerebral blood flow velocity and its impact on outcome. Ojha BK, Jha DK, Kale SS, Mehta VS. Surg Neurol. 2005 Aug; 64(2): 174-9; discussion 179.

Dr.
Prafulla Maharana
Female
Affiliation
Associate Professor
Department of
Dr. R. P. Centre for Ophthalmic Sciences
Contact
Email :
drprafulla@aiims.edu
Dr. Prafulla Kumar Maharana completed his graduation (M.B.B.S.) in 2006 from the MKCG Medical College, Berhampur, Orissa and PostGraduation in Ophthalmology (M.D.) from Dr. R.P. Centre, AIIMS, New Delhi in 2010. He has completed his senior residency in the field of cornea, cataract and refractive services from Dr. R.P. Centre, AIIMS, NewDelhi.
Hehas joined as faculty of the Dr. R.P. Centre for OphthalmicSciences in 2016and currently working as Assistant Professor of Ophthalmology in Unit-3.Previously, He has worked as Assistant Professor of Ophthalmology at AIIMS, Bhopal & AIIMS, Bhubaneswar. His areas of specialization include Cataract, Cornea and Refractive Surgery. His field of interest includes Keratoconus, Corneal infections and Keratoplasty.
He has contributedseveral chapters (19) to National and International books on ophthalmology and published 27research papers in international peer reviewed PubMed indexed journals. In addition, he has published several non-index papers.
He has been awarded Gold medal by India Academy of Pediatrics in the year 2005. He is the recipient of (as co-author) the “Best Surgical Video” by FRANZCO, Australiatwice (2002 2015) in his career.
Unit 1
Unit-2
Unit-3
Unit-4
Unit-5
Unit-6
Anesthesia and Radiology
Community Ophthalmology
Community Eye Care Services
Community Eye Care and Research Projects (Ongoing)
Eye Health Education Unit
Survey & Reports
Primary eye care clinics/Vision Centre
Ocular Biochemistry
Ocular Microbiology
Ocular Pathology
Ocular Pharmacology

Dr.
Brijesh Kr. Ratre
Male
MD
Affiliation
Assistant Professor
Department of
Onco-Anaesthesia
Contact
Email :
brajesh.ratre@gmail.com
drbrajesh@aiims.gov.in
Phone :
+91-8696156799
Area of Interest
- Special interest in Onco-Anaesthesia, Regional Techniques
- Cancer Pain Management
- Palliative Medicine
- Ultrasound guided acute and chronic pain interventions
Education and Training
| Degree/Training | Institute/University | Completion date (Month/year) /Duration | Field of Study |
|---|---|---|---|
| MBBS | Gandhi Medical College, Bhopal/ Barkatullah University, Bhopal | April 2006 | Medicine |
| MD | SMS medical College Jaipur/ Rajasthan University of Health Sciences | June 2014 | Anaesthesiology |
| CCEPC IAPC | Dr BRA IRCH, AIIMS New Delhi | December 2015 | Palliative Medicine |
| Senior Resident | Dr BRA IRCH, AIIMS New Delhi Deptt of Onco-anaesthesiology and Palliative Medicine | 31st August 2015 to 24th January 2019 | Onco-anaesthesiology and Palliative Medicine |
| Senior Resident | Deptt of Anaesthesiology, Pain and Critical Care, AIIMS, New Delhi | 25th march 2015 to 31st August 2015 | Anaesthesiology |
| Senior Resident | ESIC Model Hospital, Sector 24, Noida | 22nd July to 21st January 2015 | Anaesthesiology |
Research Experience
2011-2014 – Thesis (MD, Anes.) – “A Comparative Study of Anaesthetic Properties of Bupivacaine and Lignocaine Alone and in Combination with Clonidine And Fentanyl for Supraclavicular Brachial Plexus Block in Patients Undergoing Elective Upper Limb Surgery”
Presentations
- 2013 Podium presentation – A Comparative Study of Anaesthetic Properties of Bupivacaine and Lignocaine Alone and in Combination with Clonidine and Fentanyl for Supraclavicular Brachial Plexus Block in Patients Undergoing Elective Upper Limb Surgery at RSACPCON-2013 (National conference of Research Society of Anesthesia and Clinical Pharmacology 2013, Srinagar).
- 2013 Poster presentation – A case report: Oral teratoma in a neonate – Anesthetic challenge RSACPCON-2013 (National conference of Research Society of Anesthesia and Clinical Pharmacology 2013, Srinagar).
- 2015 Podium presentation – Comparison of properties of clonidine and fentanyl as an adjunct in supraclavicular brachial plexus block in terms of duration of post-operative analgesia A Prospective, Randomized, Double Blind Hospital based Controlled study (in ISACON 2015, Jaipur).
- 2017 Poster presentation – Multitasking team work by department of onco-anaesthesia and Palliative Medicine at International conference on Perioperative Care of Cancer Patients, 14-15 October 2017 AIIMS New Delhi.
- 2018 Podium presentation – Comparative evaluation of forced air warming & infusion of amino Acid enriched solution on intraoperative hypothermia in patients undergoing major oncological surgeries under general anesthesia : A prospective randomized study at RSACPCON-2018 (National conference of Research Society of Anesthesia and Clinical Pharmacology 2018, Jaipur).
Professional Society Membership
- 2013 Life member, Research Society of Anesthesia and Clinical Pharmacology (RSACP)
- 2015 Life member, Indian Society of Anaesthesiologist (ISA)
- 2018, Life member of Indian Association of Palliative Care
Award and Prizes
Promilajeet Virk Award (New Technique Innovation) – Second Prize During 28th National Conference of Research Society of Anaesthesiology Clinical Pharmacology RSACPCON 2018, Jaipur.
- Ratre BK, Suvvari P, Hoda W, Roychoudhury P, Bharti SJ, Bhatnagar S. Central venous catheter as peritoneal indwelling catheter for the management of recurrent malignant ascites: A case series. Indian J Palliat Care 2019;25:57-60
- Choudhary S, Dogra N, Dogra J, Jain P, Ola SK, Ratre B. Evaluation of caudal dexamethasone with ropivacaine for post-operative analgesia in paediatric herniotomies: A randomised controlled study. Indian J Anaesth 2016;60:30-3
- Prashant S, Saurabh V, Abhity G, Brajesh R, Bharti S. Peri-Operative Anesthetic Management for Low Lying Tracheal Tumor; It is all About Sharing the Surgical Field between Anesthesia and Surgical Teams: A Case Report. J Anesth Clin Res 2019;10: 899.
- Meena S, Ratre BK, Bafna U, Deganwa M. Unanticipated Difficult Intubation Caused by Unexpected Laryngeal Web in a Case of Bilateral Abductor Palsy. JCR 2014;4:367-370
- Hoda W, Ratre BK, Bharti SJ. Use of Venturi to prevent desaturation during nebulization. Lung India 2019;36:567-8
- Vadera, Hetalkumar & Mistry, Tuhin & Ratre, Brajesh. (2020). Serratus anterior plane block: Anatomical landmark-guided technique. Saudi Journal of Anaesthesia. 14. 134-135. 10.4103/sja.SJA_540_19.
- Rathore P, Kumar S, Choudhary N, Sarma R, Singh N, Haokip N, Bhopale S, Pandit A, Ratre BK, Bhatnagar S. Concerns of health-care professionals managing COVID patients under institutional isolation during COVID-19 Pandemic in India: A descriptive cross-sectional study.Indian J Palliat Care 2020;26:90-94.
- Rathore P, Kumar S, Haokip N, Ratre BK, Bhatnagar S. CARE: A holistic approach toward patients during pandemic: Through the eyes of a palliative physician. Indian J Palliat Care 2020;26:S95‐8.
- Rathore P, Kumar S, Shweta, Singh N, Krishnapriya V, Thankachan A, Haokip N, Bhopale S, Ratre BK, Bhatnagar S. A Child with Acute Lymphoblastic Leukemia in Institutional Isolation during the COVID Pandemic: A Multifaceted Responsibility. Indian J Palliat Care 2020;26, Suppl S1:170-2.
- Sirohiya P, Ratre BK. Severe acute respiratory syndrome coronavirus 2: Concerns for palliative care physicians. Indian J Pain 2020;34:143‑4.
- Sirohiya P, Ratre BK. COVID-19 pandemic and limited palliative care response: ‘‘Lack of comfort care’’.Anaesth Crit Care Pain Med (2020)
- P. Dixit et al., Ultrasound-guided central venous catheterization amid the COVID-19 outbreak:‘Revisiting protocols’,Trends in Anaesthesia and Critical Care
- Pandey K, Vig S, Ratre B, Gupta N. Use of Sterillium on Protective Goggles for Anti-Fogging during Donning for Care of COVID-19 Patients: A Novel Technique. Turk J Anaesthesiol Reanim 2020; 48(4): 344-5.
- Gupta R, Kumar V, Gupta N, Ratre BK. Perioperative management of a giant solitary fibrous tumor of Pleura. J Anaesthesiol Clin Pharmacol 2020;36:138-40